CASE REPORT
A 10-year-old girl with newly diagnosed type 1 diabetes mellitus presented with progressive deterioration of vision in both eyes within 4 weeks of diagnosis. She had a 3-month history of polyuria, polydipsia, nocturia, and generalized hair loss prior to diagnosis.
Physical and neurological examination was unremarkable. The baseline ophthalmological examination did not show any diabetic retinopathies.
However, the patient’s mother was concerned about her daughter’s loss of independence due to a rapid decline in vision. Physical examination showed visual acuity limited to the identification of color and seeing moving shadows ( hand motion vision ) due to lens opacities in both eyes.

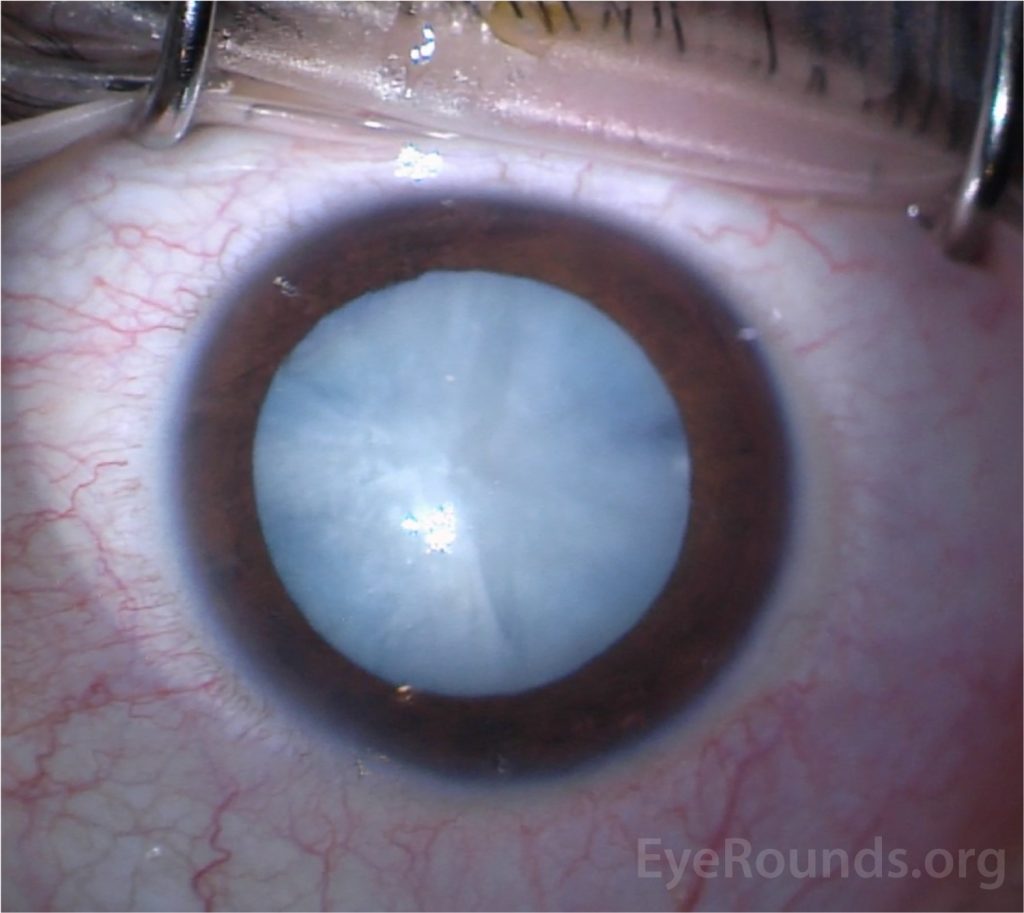
Red reflex with direct ophthalmoscope revealed blunted, whitened reflex bilaterally. Ophthalmologist confirmed the presence of bilateral dense, white cataracts.
DISEASE
A cataract is defined as the opacification of the natural crystalline lens. Cataracts are mainly age-related, but may also occur secondary to other causes such as uveitis, trauma, medications, and metabolic diseases as described elsewhere.
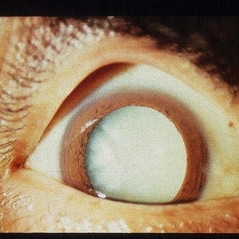
If left untreated in the long term, a cataract may advance to become an opaque, mature cataract, often causing extreme visual impairment. Mature, totally opaque cataracts prevent the organized transmission of light to the retina, rendering the patient completely blind in the affected eye.
Mature cataracts can either be dark, such as brown or black, or white. When a white cataract is termed “intumescent”, it is defined as having swelling of the lens because of epithelial impairment and fluid influx, leading to a rapid decline in visual function.
Given its surgical challenges, it is important to recognize these types of cataracts in order to achieve better outcomes during surgery.
The normal history of a cataract evolves from lens changes that are minuscule (incipient), immature, intumescent, mature corticonuclear, hypermature Morgagnian, and in its most extreme form, shrunken Morgagnian.
Patients usually present when they either have incipient or immature cataracts, so it is relatively rare to see senile intumescent and more severe forms of cataracts such as white cataracts. its higher prevalence in low socioeconomic communities reflects poor or limited access to care.
A study in India found that 8% of the total 3634 patients present with white cataracts.
Many causes can lead to senile white/intumescent cataracts including:
- Exposure to:
- Long radiation
- UV rays
- Heatwaves
- Infrared lights
- Rupture of the eye
MANAGEMENT of White cataracts
White cataracts present a high risk for complications even for inexperienced surgeons. One of the greatest challenges in managing a white cataract is the creation of a continuous circular capsulorhexis (CCC).
Studies have shown that capsulorhexis which was not totally successful in the management of white cataracts may be observed in 3.85% to 28.3% of cases with an increased incidence of posterior capsular rupture and vitreous loss.
These difficulties are mainly driven by two factors. First, the high lens density results in poor visibility given the loss of red reflex making it difficult to differentiate the edge of the anterior capsule from the white lens matter. This can be partially mitigated by using trypan staining dye but is still worse than the visibility provided when a red reflex is present.
Second, the raised intraventricular pressure causes liquified cortex escape as soon as the capsule is compromised which results in capsular tears extending to the periphery in addition to making visibility even worse. Depending on the classification, different surgical techniques may be advised.
As the OCT-based classification system was the most common, the treatments discussed will be based on those subtypes. For Type I, it is advised that the surgeon uses a single-stage forceps/needle cystotome capsulorhexis.
For Type 2, the forceps-assisted 2-stage capsulorhexis technique should be used followed by bimanual irrigation and aspiration to lower the elevated intra-lenticular pressure.
For Type 3, aspiration of the turbid fluid with needle aspiration and forceps-assisted capsulorhexis should be used. For the last type, anterior chamber decompression is needed to take out the milky fluid present with forceps-assisted capsulorhexis.
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Feldman MD B, Heersink MD S. Cataract.
- Devgan MD U. Understanding subtypes key to removing white cataracts. Healio.com.
- Brown N, Bron A. Lens disorders. Oxford: Butterworth-Heinemann; 1996.
- Rewri P, Lohan A, Aggarwal S, Chodhary P, Singhal A. Cataract surgical reach: Falling short to catch white cataracts!. Indian J Ophthalmol. 2021;69(6):1575. doi:10.4103/ijo.ijo_2560_20
- Intumescent Cataract – Symptoms, Causes, Diagnosis, Treatment & Prevention. Dr. Agarwals
- Sacu S, Ségur-Eltz N, Horvat R, Lukas J, Zehetmayer M. Intumescent cataract after topical mitomycin-C for conjunctival malignant melanoma. Am J Ophthalmol. 2003;136(2):375-377. doi:10.1016/s0002-9394(03)00207-1
- Gelender H, Gelber E. Cataract Following Radial Keratotomy. Archives of Ophthalmology. 1983;101(8):1229-1231. doi:10.1001/archopht.1983.01040020231014.
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE


