Case report of Mucormycosis
A middle-aged woman with diabetes presented to the hospital with left-sided facial pain, complete ptosis, and fever of short duration. On presentation, she had hyperglycemia without ketosis.
There was total ophthalmoplegia of the left eye with a visual acuity of 6/36. She incidentally tested positive for COVID-19.
CT paranasal sinus and MRI brain revealed left-sided pansinusitis with acute infarct in the left parieto-occipital region without angioinvasion.
An emergency functional endoscopic sinus procedure was done, which confirmed mucormycosis on histopathological examination.
Disease Entity
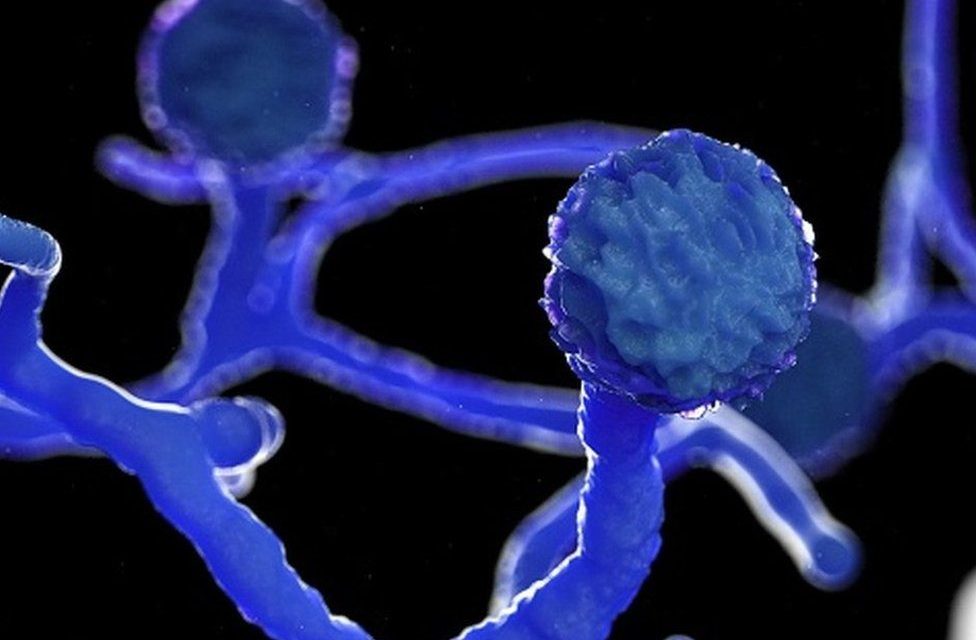
Mucormycosis, a subtype of a larger category of diseases known as zygomycoses, is an aggressive opportunistic infection that tends to show a proclivity for, among other sites (namely the lungs and gastrointestinal tract), the rhino-orbital tract.
While rhino-orbital mucormycosis is typically associated with Rhizopus species, a number of other species have also been implicated, including Mucor, Rhizomucor, Absidia, Apophysomyces, Saksenaea, Cunninghamella, Cokeromyces, and Syncephalastrum.
Epidemiology of Mucormycosis
Rhino-orbital mucormycosis tends to affect specific patient populations. It is most often associated with diabetes mellitus (type 2 more frequently than type 1, especially with a history of diabetic ketoacidosis).
Other associated conditions include neutropenia, hematologic malignancy, chronic steroid or immunosuppressive drug use, history of transplant, and history of multiple blood transfusions.
Diagnosis of Mucormycosis
 Signs and Symptoms
Signs and Symptoms
Initial symptoms of sinus-involving mucormycosis are consistent with acute or chronic sinusitis; congestion, blood-tinged secretions, rhinorrhea, headaches, fever, and malaise.
Findings of pre-septal cellulitis (soft tissue swelling, eyelid edema/erythema, and conjunctival injection) are also possible.
Involvement of the orbit is heralded by findings of chemosis, proptosis, extra-ocular motility deficits, multiple cranial neuropathies (namely CN III, V-1, V-2, and/or VI secondary to cavernous sinus involvement/thrombosis), and loss of vision.
Involvement of the contralateral eye can be an indication of extension, namely via the cavernous sinus. Development of neurologic findings such as mental status changes, seizures, or other focal neurologic deficits can indicate intra-cranial extension.

 Diagnostic procedures
Diagnostic procedures
In addition to the identification of the above clinical signs and symptoms, imaging can be helpful in diagnosis. Contrasted computed tomography (CT) of the orbits and/or paranasal sinuses can show contrast-enhancing hypodense soft-tissue thickening of the involved sinuses, most commonly the ethmoid and maxillary sinuses.
Magnetic resonance imaging (MRI) can show T2 iso-intense to hypo-intense soft tissue thickening and heterogenous post-contrast enhancement.
Boney erosion is less common but can occur. Diffusion-weighted images can show increased intensity in the affected areas secondary to restricted diffusion from infarcted mucosa.
Direct visualization of the nasal mucosa and paranasal sinuses can reveal dark, necrotic tissue and a characteristic black eschar which results from vascular invasion and tissue infarction.
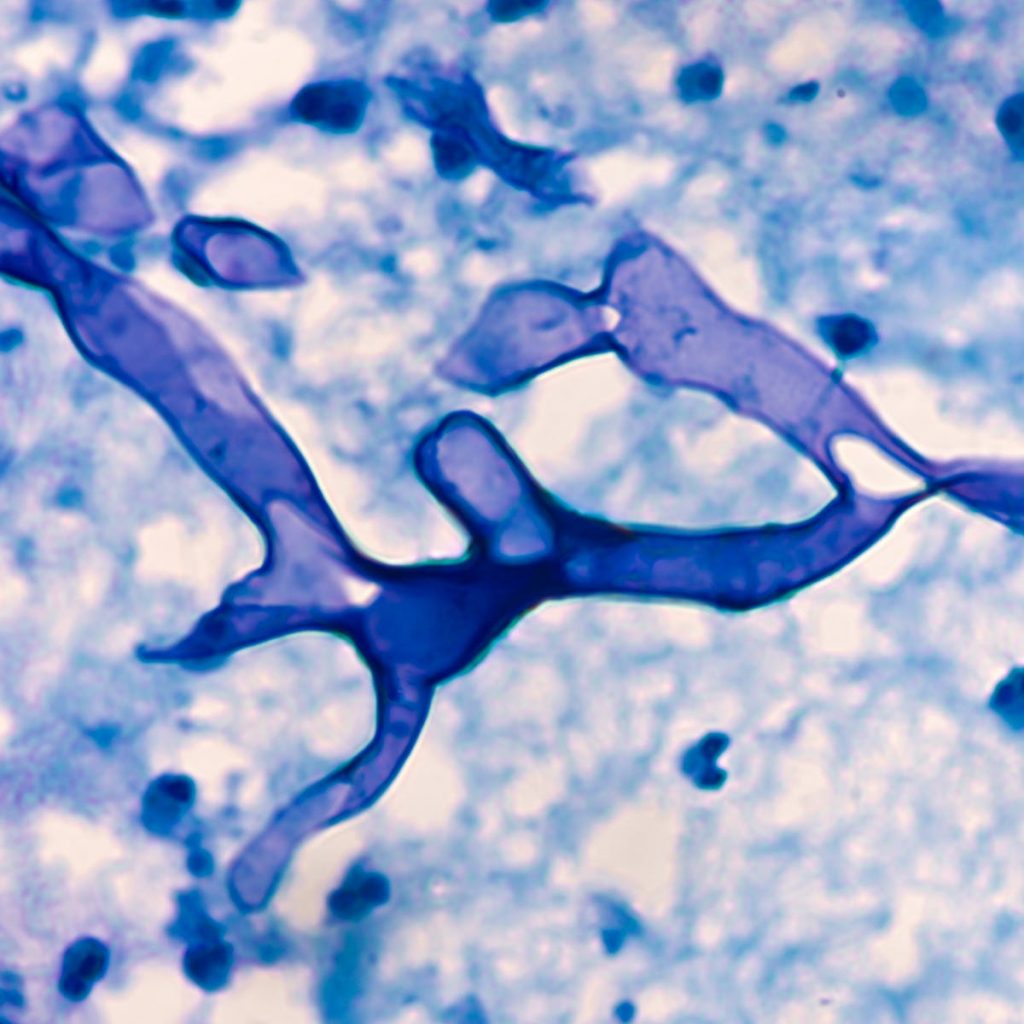
Definitive diagnosis of mucormycosis can be made via histopathologic evaluation of tissue via biopsy or scraping.
Staining of biopsy specimens with calcofluor white, periodic-acid Schiff (PAS), or Grocott-Gomori methenamine-silver stains demonstrates broad, irregular, non-septated hyphae branching at 90 degrees, which are pathognomonic for mucormycosis.
Before reading about management, let’s TAKE A BREAK … READ ABOUT SLIT-LAMP SMARTPHONE PHOTOGRAPHY
Management of Mucormycosis
 General treatment
General treatment
Early recognition and initiation of appropriate treatment are of paramount importance with regards to outcomes.
Urgent correction of underlying metabolic derangements such as hyperglycemia and metabolic ketoacidosis and tapering of corticosteroids or immunosuppressive medications should be pursued if possible.
The mainstay of medical treatment remains intravenous antifungals, namely lipid-soluble amphotericin-B at a dose of 5-7.5 mg/kg/day.
Although
older formulations of azole antifungals (fluconazole, voriconazole) have shown no efficacy in the treatment of mucormycosis, recent studies have shown some success with posaconazole as a second-line agent or in combination with amphotericin.
Additionally..
recent case reports of Mucormycosis have detailed the use of adjunctive intra-orbital irrigation with amphotericin-B (5mL of 1mg/ml daily for 7 days) in addition to intravenous therapy.
Though successful outcomes have been described, there is a paucity of large trials studying this treatment modality and its outcomes compared to the current treatment standards.
Finally..
hyperbaric oxygen (100% oxygen saturation at 2.5 – 3 ATA) and iron chelation therapy have both been described in the literature as possible adjunctive treatment modalities.
Due to the vascular compromise and tissue necrosis associated with local angio-invasion, intravenous anti-fungal agents tend to have poor tissue penetration.
Early surgical debridement of involved tissue, therefore, must be pursued. Evidence suggests that patients who do not undergo early surgical debridement had significantly higher mortality rates than those who did.
No clear guideline exists to define the extent of debridement. Extending debridement until freshly bleeding, viable tissue is encountered is a generally accepted principle.
Additionally, the use of intraoperative frozen sections to determine if clear margins have been achieved can be useful.
Prognosis of Mucormycosis
Rhino-orbital mucormycosis is a grave disease with significant mortality rates, with some published studies reporting mortality rates of up to 80% or more if untreated.
Even with prompt treatment, the prognosis remains guarded. In a series of 929 patients published in 2005, the survival rates for patients treated with amphotericin alone, surgical debridement alone, and both amphotericin and surgical debridement were 61%, 57%, and 70% respectively.
Delay treatment of Mucormycosis has been well correlated to poor outcomes, with one study showing a significant difference in survival between patients with a lag time to treatment of 7-12 days (63%) vs patients with a lag to treatment time of 13-30 days (44%).
Another study reports survival rates of 85% in patients with a lag time of 3-9 days versus just 55% in patients with a lag time of 10-45 days.
Development of hemiplegia, facial/eyelid gangrene, and cerebral invasion were all associated with a poor prognosis.

Conclusion
Rhino-orbital mucormycosis is an aggressive invasive fungal infection that tends to affect patients with a history of diabetes (especially with ketoacidosis), chronic steroid use, and immunosuppression.
Early recognition of symptoms and prompt initiation of treatment, both with intravenous antifungal agents and aggressive surgical debridement are crucial to improving clinical outcomes
Though, the prognosis for patients with this disease remains guarded even with rapid recognition and early treatment.
Read in differential diagnosis between Macroaneurysms and Coats disease.
References
- American Academy of Ophthalmology. Mucormycosis left orbit. Accessed July 27, 2020.
- Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, Sein M, Sein T, Chiou CC, Chu JH, Kontoyiannis DP, Walsh TJ. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41:634–653
- Ribes JA, Vanover-sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000;13(2):236-301.
- Kasapoglu F, Coskun H, Ozmen OA, Akalin H, Ener B. Acute invasive fungal rhinosinusitis: evaluation of 26 patients treated with endonasal or open surgical procedures. Otolaryngol Head Neck Surg. 2010;143(5):614-20.
- Yohai RA, Bullock JD, Aziz AA, Markert RJ. Survival factors in rhino-orbital-cerebral mucormycosis. Surv Ophthalmol. 1994;39(1):3-22.
- Karadeniz uğurlu Ş, Selim S, Kopar A, Songu M. Rhino-orbital Mucormycosis: Clinical Findings and Treatment Outcomes of Four Cases. Turk J Ophthalmol. 2015;45(4):169-174
- Gamaletsou MN, Sipsas NV, Roilides E, Walsh TJ. Rhino-orbital-cerebral mucormycosis. Curr Infect Dis Rep. 2012;14(4):423-34
- Therakathu, J., Prabhu, S., Irodi, A., Sudhakar, S.V., Yadav, V.K., Rupa, V. Imaging features of rhinocerebral mucormycosis: A study of 43 patients. Egyptian Journal of Radiology and Nuclear Medicine 2018; 49(2) 447-452.
Read more about: Cornea Verticillate, Tadpole Pupil, Choroidal Folds

RETINAL IMAGING BY YOUR SMARTPHONE