DISEASE
Shaken Baby Syndrome (SBS) is one form of physical child abuse, a non-accidental traumatic brain injury. It is included in the abusive head trauma classification.
In 6% of reported cases of child abuse, an ophthalmologist is responsible for initially recognizing the abuse. Retinal findings may be the only manifestation of this abuse. It is a diagnosis that has important medical-legal implications.
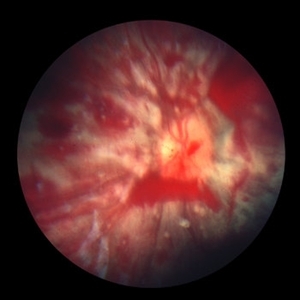
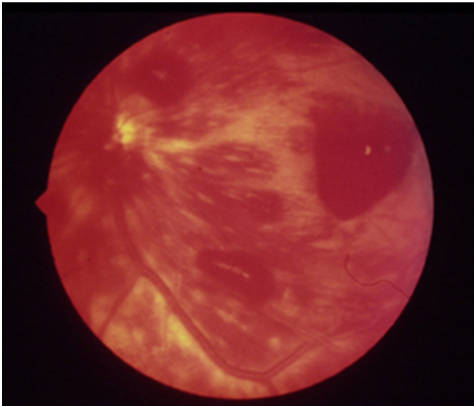
Retinal hemorrhages are the cardinal manifestation of SBS. The incidence of retinal hemorrhages in SBS is approximately 85%. Classically, children with SBS have retinal hemorrhages which are multilayered – preretinal, intraretinal, and subretinal.
They are usually too numerous to count and extend out to the retinal periphery (i.e. not just confined to the posterior pole). Macular retinoschisis (splitting of the retinal layers) may also be associated with SBS.
As retinal hemorrhages may subside over time, prompt retinal photography is recommended at the time of discovery of retinal hemorrhages on dilated funduscopic exam to document findings as a baseline for future comparison.
If possible, extended ophthalmoscopy with examination of the entire retina with scleral depression is recommended to also evaluate for peripheral nonperfusion (from retinal vascular disruptions) and neovascularization as well as for peripheral retinal tears, hemorrhages, and other pathology.

If possible, wide-sweeping photographs and fluorescein angiography are recommended as soon as the discovery of retinal hemorrhages from SBS / NAT are discovered. Examination under anesthesia may be required to obtain imaging as well as administer treatment.
MANAGEMENT
Overall, prevention is the best therapy. Many hospitals and healthcare centers offer classes and education on how to cope with the stresses of parenthood.
Unfortunately, some children will require treatment for amblyopia or strabismus. Patching therapy and glasses may be needed to treat the amblyopia induced by the ocular trauma.
If preretinal blood obscures the macula raising concern for amblyopia, several options can be tried. One is maintaining the infant upright during the day if possible given other comorbidities. Upright positioning allows the blood to settle inferiorly within the bleb and may allow the fovea to be sufficiently clear to avoid surgical evacuation.
Surgical vitrectomy may be needed for non-clearing vitreous hemorrhage, macular hole, or retinal detachment, but procedures are complex in infants’ eyes and often require consultation with a pediatric retina-trained surgeon.
Often, the prognosis can vary significantly for victims of SBS depending on the severity of the trauma and effect on the central neural system. Careful physician documentation of findings and fundus photography can prove very helpful, especially in a court of law.
Retina photographs with wide-sweeping fluorescein angiography are recommended to document baseline intraretinal hemorrhages and other pathologic changes as described above as well as to evaluate for peripheral nonperfusion and possible neovascularization development.
Peripheral nonperfusion may lead to development of neovascular tissue that subsequently may contribute to vitreous hemorrhage and tractional or complex tractional/rhegmatogenous retinal detachment.

If significant peripheral nonperfusion is detected, peripheral scatter laser to all regions of nonperfusion may be considered to reduce the risk of neovascularization and subsequent retinal detachment.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Caputo G. and Wu Wei-Chi. Nonoaccidental Head Trauma. In Pediatric Retina, third edition. Hartnett, ME Editor-in-Chief. Wolters Kluwer Philadelpha PA 2021.
- Friendly DS. Ocular manifestations of physical child abuse. Trans Am Acad Ophthalmol Otolaryngol 1971; 75: 318-332.
- Newton AW, Vandeven AM. Update on child maltreatment with a special focus on shaken baby syndrome. Curr Opin Pediatr 2005; 17: 246-251.
- Sternberg P Jr. Trauma: principles and techniques of treatment. In: Ryan SJ, ed. Retina, 2ndedn, vol. 3. St. Louis: Mosby; 1994: 2351-2378.
- Kivlin J, Simons K, Lazoritz S, Ruttum M. Shaken baby syndrome. Ophthalmology. 2000; 107(7): 1245-1254.
- Greenwald, Weiss, Oestrerle, Friendly. Traumatic retinoschisis in battered babies. Ophthalmology. 1986; 93(5): 618-625.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

