CASE REPORT
Case report of Cogan’s syndrome 64-year-old computer analyst, presenting with a six-week history of malaise, a stone in weight loss. He had a three-week history of fevers and sweats, headaches, and a painful elbow.
He had developed acute hearing loss, poor balance, and a rash across his chest and ankles. There was no travel history, sexual history, or contact with unwell individuals.

Examination revealed a temperature of 38 degrees Celsius, a sparse petechial rash across his chest and shins, no joint swellings, lymphadenopathy, or organomegaly.
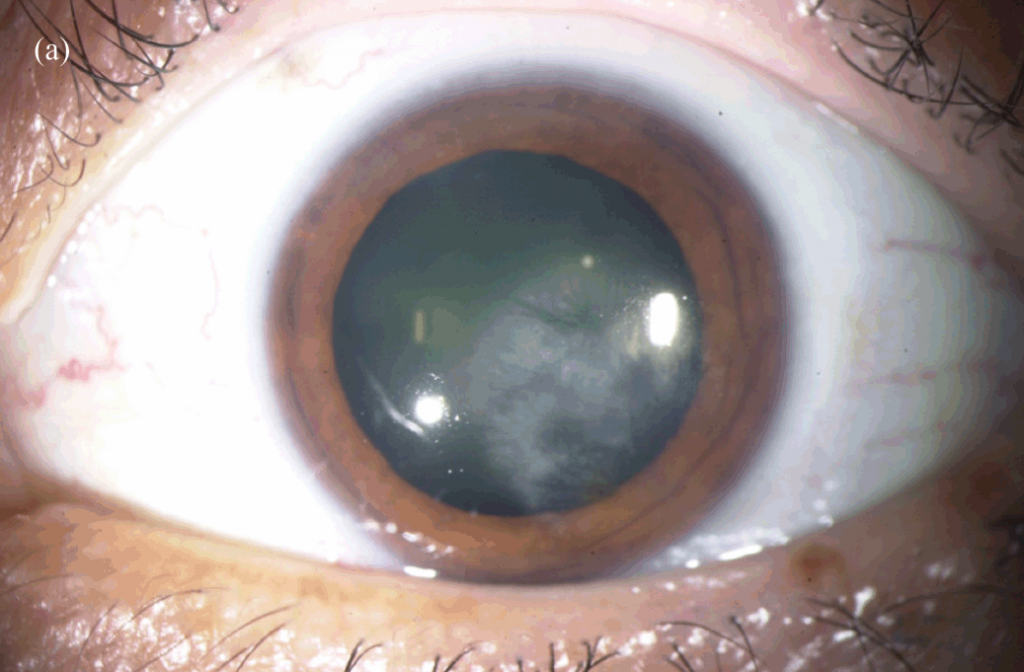
Slit-lamp examination demonstrated nodular scleritis. External auditory canal examination was normal, and a sensorineural pattern of hearing loss was detected.
Results: Investigations revealed a hemoglobin of 123 g/l (normocytic), a white cell count of 16.80 109/l, neutrophils 15.02 109/l, and a CRP of 284 mg/l. Urinalysis was normal. Blood and urine cultures were negative. Serology for hepatitis, HIV, and syphilis was negative.
ANA, ANCA, and RF testing were negative. Immunoglobulin and complement levels were normal. A CT brain was normal, and a CT angiogram of the aorta and mesenteric vessels showed no changes suggestive of vasculitis.
The rash was transient and faded before a biopsy was obtained. Audiograms confirmed bilateral sensorineural hearing loss. A clinical diagnosis of Cogan’s syndrome was made.
DISEASE of Cogan’s syndrome
Cogan’s syndrome (also Cogan syndrome) is an uncommon disease seen mostly in young adults that can severely affect vision and hearing. Since 1945, only several hundred cases have been reported in the literature.
Cogan syndrome is characterized by recurrent ocular inflammation as well as hearing loss that can lead to deafness if left untreated.
Systemic involvement can be seen in up to 80% of patients. Hearing loss, headache, arthralgia, fever, arthritis, and myalgias are the most common systemic symptoms of Cogan syndrome, and up to 15% of patients develop vasculitis.
Cogan syndrome can also lead to cardiovascular complications such as aoritis, as well as gastrointestinal and neurologic manifestations.
Cogan syndrome most commonly affects young adults between 20-30 years old but can be seen at any age, and while the etiology is unknown, infectious triggers, such as upper respiratory tract infection, diarrhea, dental infection, or recent immunization have been reported.
MANAGEMENT of Cogan’s syndrome
Patients with Cogan syndrome should be monitored closely and managed by ophthalmologists, internists, and otolaryngologists. Treatment of Cogan syndrome depends on the severity and the degree of systemic involvement.
Cogan syndrome is typically treated with steroids. Topical corticosteroids, cycloplegics, and disease-modifying anti-rheumatic drugs (DMARDS) can be used to manage acute interstitial keratitis.
However,
one must exercise caution when treating with steroids for ocular inflammation because it could lead to elevated intraocular pressure or premature formation of cataracts. Topical Cyclosporin A may be effective in treating severe anterior segment inflammation in the setting of Cogan syndrome.
Systemic corticosteroids may be considered (1-2mg/kg/day for 2-6 months) after the onset of hearing loss or when there is posterior involvement of the eye, such as retinal vasculitis, posterior scleritis, and posterior uveitis.
In addition, involvement of the inner ear, severe eye involvement, or development of systemic vasculitis may necessitate aggressive immunosuppressive therapy. When a patient does not respond to steroids or there is a contraindication to steroid use, DMARDs or biologic agents are recommended.
Infliximab is now commonly used along with corticosteroids, especially in those who have failed combinations of steroids and DMARD therapy. This allows for tapering of corticosteroids in 86% of patients.
More about syndromes such as Aicardi syndrome, Branch Retinal Artery Occlusion, Arlt’s Triangle, Tadpole Pupil, Plateau Iris
HOW TO TAKE SLIT-LAMP EXAM IMAGES BY A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which the photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adaptors.
REFERENCES
- Espinoza, Gabriela Mabel, et al. “Cogan’s Syndrome: Clinical Presentations and Update on Treatment.” Current Allergy and Asthma Reports, vol. 20, no. 9, 16 June 2020, doi:10.1007/s11882-020-00945-1.
- Haynes, Barton F., et al. “Cogan Syndrome.” Medicine, vol. 59, no. 6, 1980, pp. 426–441., doi:10.1097/00005792-198011000-00003.
- Durtette, Charlotte, et al. “Cogan Syndrome: Characteristics, Outcome, and Treatment in a French Nationwide Retrospective Study and Literature Review.” Autoimmunity Reviews, vol. 16, no. 12, 2017, pp. 1219–1223., doi:10.1016/j.autrev.2017.10.005.
- Orsoni, Jelka G., et al. “Cogan Syndrome.” Cornea, vol. 21, no. 4, 2002, pp. 356–359., doi:10.1097/00003226-200205000-00005.

RETINAL IMAGING BY YOUR SMARTPHONE



