CASE REPORT
A 55-year-old male patient underwent uneventful clear corneal phacoemulsification and in-the-bag IOL implantation in the right eye (OD).
Medical records showed postoperative visual acuity of 6/6, N6 OD. He presented to us three years after surgery with complaints of a mild dimness of vision (6/12, N8) and seeing cob-web-like matter in his right eye of two weeks duration.
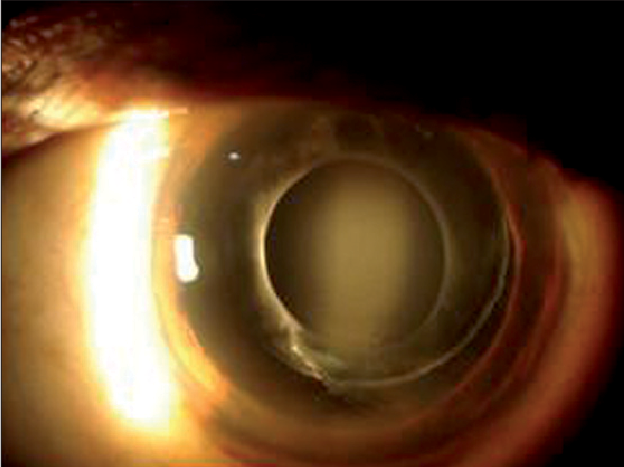
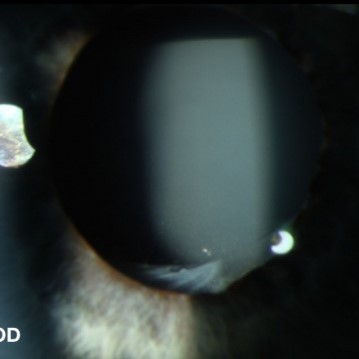
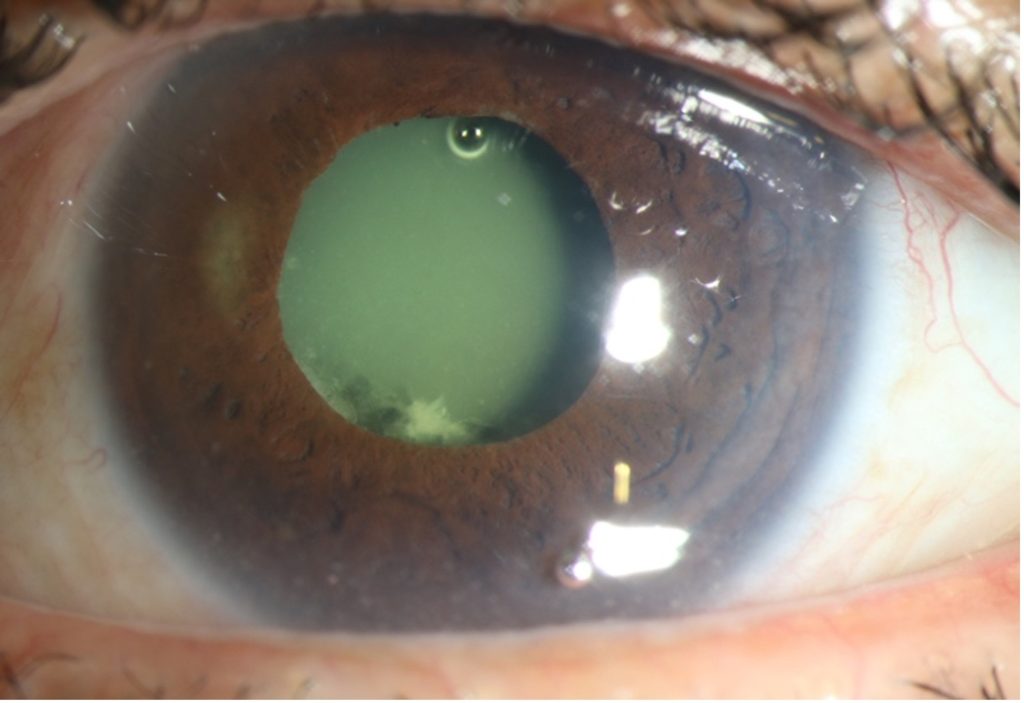
Slit lamp examination OD showed a normal anterior chamber and a well-centered in-the-bag IOL. There was posterior bowing of the posterior lens capsule with the accumulation of turbid fluid in the space between the IOL and the capsule.
Ultrasound biomicroscopic examination (UBM) confirmed the findings. The intraocular pressure was 18 mm of Hg in both eyes. Fundus examination was normal. A diagnosis of Capsular Bag Distension Syndrome (CBDS) was made.
Capsular Bag Distension Syndrome (CBDS) entity
Capsular bag distension syndrome (CBDS) (i.e. capsular block syndrome, capsular bag hyper distension, capsulorhexis block syndrome) is a rare complication of cataract surgery within the bag intraocular lens placement where turbid fluid builds up in between the intraocular lens and posterior capsule, eventually leading to a decline in visual acuity for the patient.
One study estimates the occurrence of CBDS to occur in less than 1% (0.73%) of patients undergoing phacoemulsification with posterior chamber intraocular lens (PCIOL) implantation. The presentation can occur within a few weeks to months, or even years, after cataract surgery.
One large retrospective study found that eyes with axial lengths greater than 25 mm were at greater risk for CBDS. Patients receiving four-haptic PCIOLs, compared to C-loop IOLs, were also found to be at greater risk. Almost all cases are associated with continuous curvilinear capsulorhexis with an overlap all over the anterior surface of the optic.
Capsular Bag Distension Syndrome (CBDS) MANAGEMENT
General treatment
Treatment most commonly entails Nd: YAG laser posterior and/or anterior capsulotomy. YAG allows for quick release of the trapped fluid and returns the IOL to its previous position, resolving the patient’s myopic shift and visual blurring.
Openings are most commonly made in the posterior capsule. However, if the posterior capsule is clear one can elect to create a small opening in the anterior capsule just peripheral to the edge of the lens implant, after which fluid will vent into the anterior chamber where it is quickly cleared through normal aqueous humor turnover.
If this latter approach is taken, some clinicians recommend a short course of topical steroids due to the higher risk of post-op inflammation. The liberated lens matters may also cause an increase in intraocular pressure which, however, usually responds to medical therapy.
In early, asymptomatic cases clinicians can also elect to observe. If cortical masses protruding from the anterior capsule lead to inflammation, topical anti-inflammatory medications can be utilized and surgical aspiration may be necessary or even pars plana vitrectomy with posterior capsulotomy.
If P. acnes chronic endophthalmitis is suspected in conjunction with CBDS, pars plana vitrectomy, removal of the debris as much as possible and total capsulotomy may be necessary.
Vlasenko et al. recommends the following treatments for the previously mentioned CBDS types:
- Type 1: Follow-up
- Type 2: If symptomatic, YAG Capsulotomy; if not, observe
- Type 3: YAG Capsulotomy
- Type 4: YAG Capsulotomy, unless inflammatory symptoms develop, then consider topical anti-inflammatories and surgical aspiration
Some surgeons advocate bimanual irrigation and aspiration for all cases of late CBDS, with the logic being that this allows the culture of the fluid to test for P. acnes as well as prevent the spread of any bacterium into the vitreous cavity.
Indeed, cases of P. acnes endophthalmitis have been noted after simple YAG capsulotomy without the presence of any turbid fluid from CBDS. In one reported case of bimanual irrigation and aspiration for CBDS where culture revealed P. acnes, no anterior chamber cell, and flare was seen on the pre-operative exam.
However, these cases are exceedingly rare and most surgeons, in the absence of any inflammatory symptoms or signs, elect for simple YAG capsulotomy.
Surgical follow-up
Clinicians should watch for post-operative inflammation as rare cases of P. acnes endophthalmitis have been reported following Nd: YAG treatment for other indications, possibly due to the release of a sequestered low-virulent organism.
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Kim HK, et al. Capsular block syndrome after cataract surgery: clinical analysis and classification. J Cataract Refract Surg. 2008;34:357–63.
- Burk, R. Capsular Bag Distension Syndrome. 12 January 2015.
- Killoran E, Haugsdal J, Oetting TA. Capsular Block Syndrome: An Unusual Presentation. EyeRounds.org. July 6, 2016.
- Vlasenko A, Malyugin B, Verzin A, Uzunyan D. Capsular bag distention syndrome: case series and management strategies. European Society of cataract and refractive surgeons. 10 October 2017.
- Wendrix G, Zeyen T. Late-onset capsular bag distension syndrome after cataract surgery: 2 case- reports. Bull Soc Belge Ophtalmol. 2006;301:67–9.
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE

