DISEASE
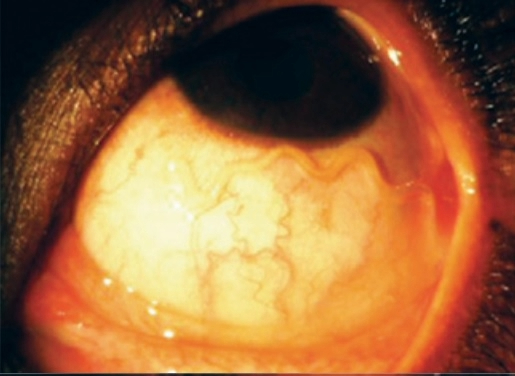
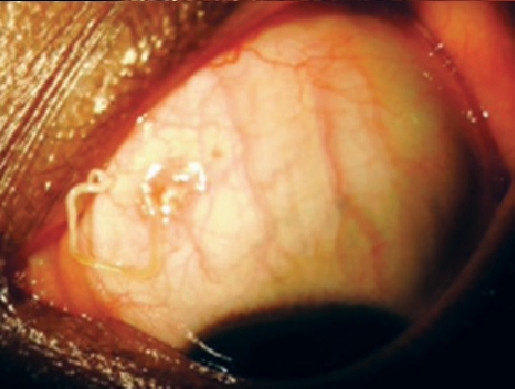
Loa Loa Filariasis is an infection of the submucosal and subcutaneous tissue caused by the filarial nematode Loa loa. Eyeworm is a pathognomonic finding in the disease course and occurs when the adult worm is visualized migrating beneath the bulbar conjunctiva.
Cutaneous manifestations including Calabar swellings are also pathognomonic and are likely due to a hypersensitivity response elicited by migration of the adult worm through tissue.
Loiasis has traditionally been regarded as a benign condition. A primary cause for concern has been the risk for encephalopathy and other severe adverse reactions when ivermectin is administered to individuals who are coinfected with Loa loa and Onchocerca volvulus.
However, the view of loiasis as a benign disease has been called into question by the finding that the population-attributable fraction of mortality associated with Loa loa microfilaremia is 14.5%.
It is hypothesized that this increased risk of mortality is due to obstructive or inflammatory processes within the circulation.
This theory also explains the mechanism of retinal vessel involvement in Loa loa retinopathy, and might readily be applied to other organ systems.
Loa loa is transmitted by the deerfly of the Chrysops genus, which demonstrates a diurnal pattern of activity, being most active from 10 am – 2 pm.
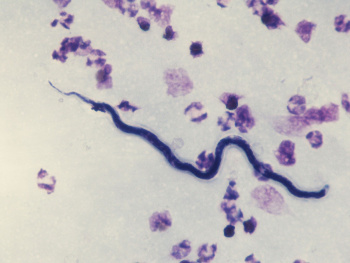
Microfilariae are sheathed and can be found in the spinal fluid, urine, sputum, lungs, and blood of an infected individual.
Their diurnal activity coincides with that of the Chrysops fly, increasing their likelihood of ingestion during a blood meal.
The microfilariae mature through the third larval stage (L3) within the fly, migrate to the proboscis, and enter a new host via a subsequent blood meal, where they mature into adult nematodes.
Once within the human host, the maturation process from L3 larvae to adult nematode is estimated to require 150-170 days. Disease manifestations, therefore, may not occur until 6-18 months from the time of inoculation.
Diagnosis
Definitive diagnosis of loiasis is made by detection of the worm in the subconjunctiva of the eye or visualization of microfilariae on a blood smear in a patient from an endemic region or who has traveled to a high-risk area.
Surgical removal of the worm from the subconjunctival space allows for laboratory identification of the species. Calabar swellings may also help to confirm the diagnosis.
Ophthalmic Signs and Symptoms
Loa loa is referred to as “African Eye Worm” because it can be observed migrating across the periorbital tissues and into the subconjunctiva.
This observation is not associated with lasting damage to tissues. However, discomfort and foreign body sensations are commonly reported symptoms.
MANAGEMENT
Medical therapy
Pharmacotherapy is the preferred treatment of loiasis, as high systemic microfilarial loads mean that surgical intervention is not capable of eradicating the infection.
When microfilarial loads are beneath a suggested threshold of 2500 mg/mL blood, diethylcarbamazine (DEC) remains the first-line treatment for loiasis.
It is prescribed as 8-10 mg/kg three times per day for three weeks. DEC demonstrates efficacy against both adult worms and microfilariae and provides effective prophylaxis for individuals visiting endemic regions.
DEC is contraindicated in patients coinfected with onchocerciasis due to the risk of Mazzotti reaction, which consists of fever, tachycardia, hypotension, arthralgia, and adenitis accompanied by anterior and posterior segment inflammation when the eye is involved.
It is caused by migration of the worms from the dermis into the vasculature and cerebrospinal fluid due to DEC therapy, where degradation results in a disseminated inflammatory response which can be fatal.
The severity of the reaction is correlated with pretreatment microfilarial load as demonstrated by skin snip.
Similarly, the major complication of medical treatment for loiasis is a serious adverse reaction resulting in encephalopathy and retinal hemorrhage due to the sudden killing of microfilariae when present in high numbers in the blood.
Albendazole is used as sequence therapy for patients with microfilarial loads greater than 2500 mf/mL blood, as it targets adult worms but not microfilariae and thereby reduces blood counts slowly.
Because it more gradually decreases microfilarial loads, it is associated with fewer adverse effects compared to DEC. Albendazole may also be used as adjunct therapy in cases refractory to multiple treatments with DEC.
Ivermectin is highly effective against L. loa, and a single dose can reduce systemic microfilarial loads for over a year. However, it has no activity against adult worms.
Pretreatment with albendazole may be appropriate in patients with a high microfilarial load, as pharmacotherapy with ivermectin has been demonstrated to cause serious neurological adverse events in these patients.
The first signs occur within 12-24 hours following treatment and include fatigue, generalized arthralgia, agitation, mutism, and incontinence.
Later signs include coma and loss of consciousness and manifest 24-72 hours post-treatment. Ophthalmic findings include retinal and conjunctival hemorrhage. The risk for this syndrome is associated with significant microfilaremia.
Medical follow up
Patients should be followed closely for the first three days after initiation of DEC therapy for concern of Mazzotti reaction, a systemic reaction that includes fever, malaise, and lymphadeopathy.
Albendazole has not been demonstrated to cause any adverse reactions when initiated for pretreatment. Patients ought to be evaluated throughout their three-week course.
Failure to reduce microfilarial loads by the end of the three-week treatment course warrants additional courses of therapy or a switch to a different class of drug.
Surgery
Surgical removal of adult worms from the conjunctiva of the eye is indicated whenever the adult worm presents in the subconjunctival space and is followed up with systemic medications, which prevent recurrence by reducing systemic micro- and macrofilarial loads.
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Passos RM, Barbosa CP, Almeida Jde S, Ogawa GM, Camargo LM. Subconjunctival Loa loa worm: first case report in Brazil. Arq Bras Oftalmol. 2012 Jan-Feb;75(1):67–70. pmid:22552423
- Padgett JJ, Jacobsen KH. Loiasis: African eye worm. Trans R Soc Trop Med Hyg 2008; 102(10): 983-9.
- Whittaker C, Walker M, Pion SDS, Chesnais CB, Boussinesq M, Basanez MG. The Population Biology and Transmission Dynamics of Loa loa. Trends Parasitol 2018; 34(4): 335-50.
- Herrick JA, Metenou S, Makiya MA, et al. Eosinophil-associated processes underlie differences in clinical presentation of loiasis between temporary residents and those indigenous to Loa-endemic areas. Clin Infect Dis 2015; 60(1): 55-63.
- Boussinesq M. Loiasis. Ann Trop Med Parasitol 2006; 100(8): 715-31.
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE

