Ocular cicatricial pemphigoid (OCP) poses a unique management challenge to eye care practitioners and often requires a multidisciplinary approach between dry eye, uveitis, and oculoplastic specialists.
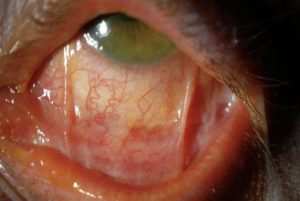
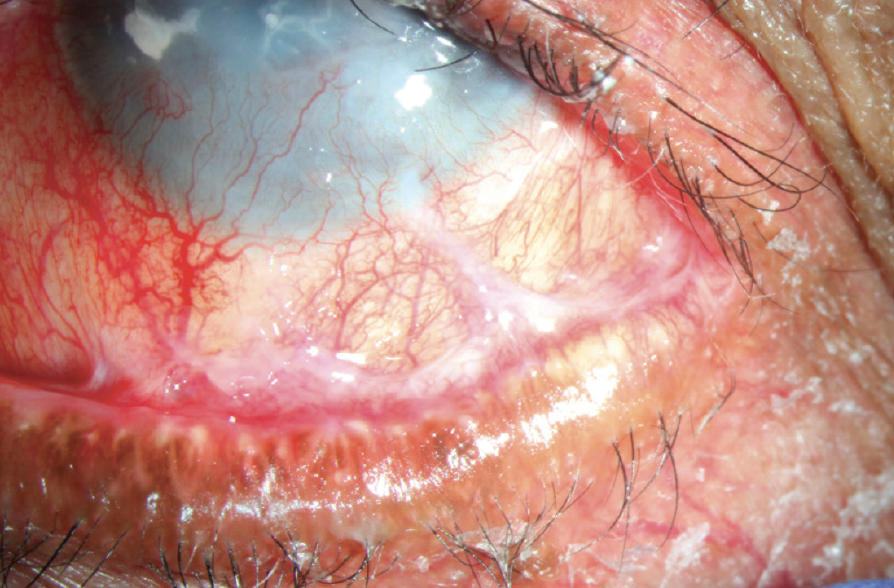
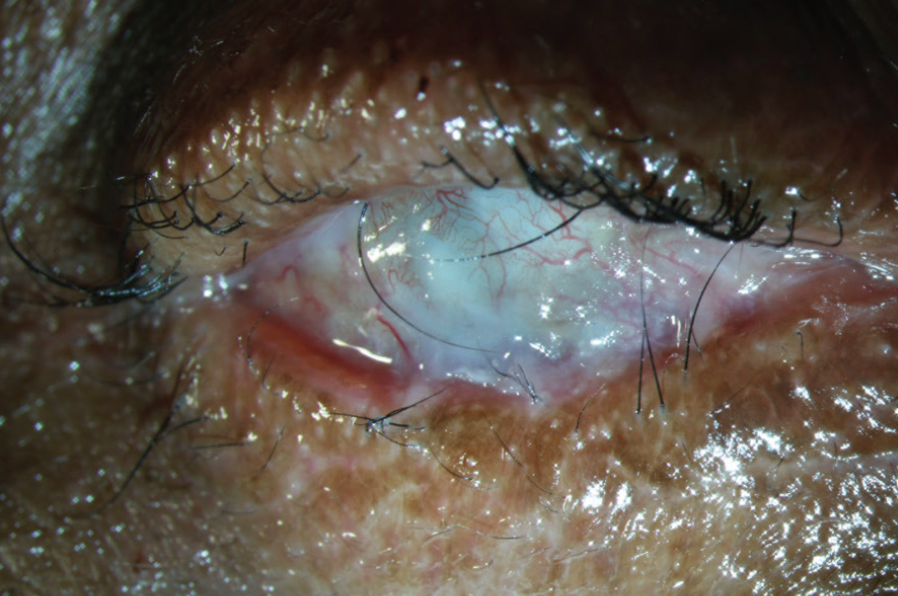
This cicatrizing conjunctivitis results in an abnormal ocular surface and eyelid anatomy, leading to an unstable tear reservoir, reduced tear drainage, poor blink mechanics, exposure keratopathy, and cicatricial entropion with trichiasis.
Understanding the disease process is crucial to effectively managing ocular surface disease (OSD) related to Ocular cicatricial pemphigoid (OCP).
OCP is a systemic autoimmune inflammatory disease and is a subset of mucous membrane pemphigoid (MMP) that occurs in 1/10,000 to 1/50,000 individuals.
It disproportionately affects women at a ratio of approximately 2:1 with no racial predilection.2 The linear deposition of immunoglobulin (Ig) A, IgC, and C3 in the epithelial basement membrane of the conjunctiva characterizes the disease.
This deposition results in conjunctival scarring, inferior fornix shortening, and symblepharon. Conjunctival scarring may also cause cicatricial entropion and trichiasis, and in later stages, vision loss may occur due to limbal stem cell deficiency and central corneal opacification. End-stage OCP includes ankyloblepharon.
Read more about OCULAR CICATRICIAL PEMPHIGOID (OCP) Disease entity and diagnosis
Treatment
In untreated cases, the disease progresses in about 75% of patients. Although systemic treatment halts cicatrization progression for most patients, it is ineffective for around 10% of them.
Ocular involvement in OCP poses a significant risk subset of MMP and typically requires systemic therapy alongside topical treatment.
Managing systemic treatment should be overseen by a physician with expertise in anti-inflammatory and immunomodulatory treatment due to potential systemic complications, necessitating regular blood tests.
Various drugs are effective for treating Ocular cicatricial pemphigoid (OCP), with a recommended step-wise approach for escalating therapy in cases of inadequate response.
While topical therapy can aid in managing surface symptoms, it should not replace systemic treatment. This includes optimizing ocular surface lubrication with artificial tears and punctal plugging.
Although topical and subconjunctival steroids can alleviate symptoms, they do not address the underlying disease.
While topical cyclosporine has shown limited effectiveness, topical tacrolimus has demonstrated success in small case studies. Subconjunctival mitomycin-c has been explored with varying results in small case series.
If the disease remains inactive after a few years of systemic therapy, discontinuing systemic treatment may be possible for many patients. However, ongoing monitoring is crucial as up to 22% of patients may experience disease recurrence.
Mild Disease:
Dapsone is an effective and commonly used anti-inflammatory treatment in Ocular cicatricial pemphigoid (OCP) for mild disease and in the absence of rapid progression.
Dapsone is started at a dose of 50 mg/day and slowly increased as tolerated by up to 25mg every 7 days to an effective dose, which is usually between 100-200mg/day.
If significant improvement is not achieved within 3 months, escalation of therapy is recommended such as to azathioprine or methotrexate.
Systemic complications of dapsone include hemolysis and methemoglobinemia. G6PD (glucose-6-phosphate dehydrogenase) deficiency is a contraindication to dapsone therapy as dapsone can precipitate a hemolytic crisis.
All patients should be screened for G6PD deficiency before initiation of therapy with dapsone.
Moderate to Severe Disease:
Corticosteroids have a rapid effect and are useful during the acute phase of severe or rapidly progressive disease.
Adjuvant corticosteroid-sparing immunomodulatory therapy should be initiated simultaneously as it may take weeks to become therapeutic.
This will allow a quicker taper from steroids and the shortest course of steroid therapy necessary given the significant systemic side effects of long-term steroid therapy.
Generally, once quiescence is achieved, steroids are tapered slowly. Screening for tuberculosis (TB) is recommended prior to the initiation of steroid therapy.
Azathioprine has been shown to be an effective steroid-sparing therapy. It takes 8-12 weeks of treatment to achieve maximal effect and thus should be used initially concurrently with steroids.
Screening for thiopurine methyltransferase (TPMT) deficiency is recommended prior to initiation of azathioprine as TPMT-deficient patients are at higher risk of developing myelosuppression.
Systemic complications include leukopenia, pancytopenia, infection, malignancy, and drug-induced hypersensitivity syndrome.
Methotrexate has been shown to be an effective monotherapy for Ocular cicatricial pemphigoid (OCP) with fewer adverse effects when compared to azathioprine, cyclophosphamide, and dapsone.
The Systemic Immunosuppressive Therapy for Eye Diseases (SITE) trial found that cyclophosphamide was effective in controlling inflammation in 70.7% of patients with OCP at 1 year, with 66.9% of patients on less than or equal to 10mg of prednisone.
Low-dose methotrexate is particularly effective in mild to moderate Ocular cicatricial pemphigoid (OCP). Systemic complications include hepatotoxicity, nephrotoxicity, pneumonitis, pulmonary fibrosis, pancytopenia, and malignancy.
Tetracyclines are a well-tolerated anti-inflammatory agent and have been found to be effective for mild to moderate OCP, particularly when combined with nicotinamide.
Mycophenolate mofetil has been shown to be a well-tolerated and effective therapy for OCP. Therapeutic dosage is usually 1000-2000mg/day. Systemic complications include leukopenia.
Cyclosporine has only been used in a small series of patients and has been reported to have variable levels of effectiveness.
Severe Disease:
Cyclophosphamide is the first line in patients with severe disease or rapid progression. It should be started in conjunction with steroids and can be dosed orally or IV.
A short course of pulsed IV therapy (ex. 3 days) can be particularly effective in achieving rapid control if needed, such as prior to surgery.
The SITE trial found that cyclophosphamide was effective in controlling inflammation in 80.8% of patients with OCP at 1 year, with 58.5% of patients on less than or equal to 10mg of prednisone. Systemic complications include myelosuppression, carcinogenesis, and teratogenicity.
Intravenous Immunoglobulin (IVIG) is reserved for patients with progressive disease that is unresponsive to systemic steroids and cyclophosphamide and has been found to be an effective therapy.
Dosing is every 3-4 weeks until quiescence is achieved, usually requiring 4-12 cycles. Systemic complications are severe and include anaphylaxis, disseminated intravascular coagulation (DIC), aseptic meningitis, and acute renal failure. Therefore, IVIG is which is reserved for refractory disease.
Biologics, including the anti-TNF agents Etanercept and infliximab, the IL-2 antagonist daclizumab, and the anti-CD20 antibody rituximab have been shown to be efficacious in small studies of patients with refractory OCP.
The combination of IVIG and rituximab has been shown to be effective as well in refractory Ocular cicatricial pemphigoid (OCP).
Complications
Seemingly trivial surgical intervention and conjunctival trauma can lead to serious exacerbation of disease.
Surgical intervention, such as treatment of trichiasis, entropion, and cataracts should be deferred if possible until control of active disease is achieved. In some situations, this may not be possible and a multi-disciplinary approach is best.
Inferior eyelid retractor plication for trichiasis avoids surgery on the conjunctiva and has been shown to be safe and effective when undertaken in the setting of clinically quiescent Ocular cicatricial pemphigoid (OCP).
Cryotherapy for the treatment of trichiasis has also been shown to be safe and moderately effective when undertaken in the setting of clinically quiescent OCP.
In a case series of patients with well-controlled OCP undergoing entropion repair, successful repair was performed in all patients regardless of the type of surgery.
Safe and successful performance of cataract surgery has been shown in several case series of patients with well-controlled OCP. A clear corneal incision is recommended to reduce the risk of exacerbation.
Glaucoma is also a possible complication of Ocular cicatricial pemphigoid (OCP) and is particularly difficult to diagnose and treat. IOP measurements are unreliable, and examination and ancillary testing are limited by ocular surface disease.
A case series of 61 patients with severe OCP found that 21% of patients also had glaucoma and an additional 9% developed glaucoma over the course of the follow-up.
OCP has been described in patients with other concurrent rheumatologic illnesses including rheumatoid arthritis, lupus, and HLA-B27 spondyloarthropathies.
Future directions
Membrane array testing of specific tear proteins testing may be a potential method of monitoring response to therapy.
Using a membrane array kit purchased from RayBiotech Inc, Chan et al tested 43 angiogenic modulators and found elevated levels of IL-8 and MMP-9 in the tears of patients with OCP, and these levels decreased with systemic immune therapy.
Arafat et al proposed MPO levels in tears as a sensitive and specific quantitative marker of disease activity.
Cultivated oral mucosal epithelial transplantation has been shown to be effective in the treatment of ocular surface disease secondary to limbal stem cell deficiency (including OCP) and is a promising avenue of treatment.
A keratoprosthesis or osteo-odonto-keratoprosthesis can be used for visual rehabilitation in severe end-stage disease and is an active area of ongoing research.
The Boston keratoprosthesis type I has been found to have less favorable clinical outcomes when compared to implantation of the Boston keratoprosthesis type II in OCP.
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
References
- Gibbons A, Johnson TE, Wester ST, et al. Management of Patients with Confirmed and Presumed Mucous Membrane Pemphigoid Undergoing Entropion Repair. Am J Ophthalmol. 2015;159(5):846–852.
- Puranik CJ, Murthy SI, Taneja M, Sangwan VS. Outcomes of cataract surgery in ocular cicatricial pemphigoid. Ocul Immunol Inflamm. 2013;21(6):449-54.
- Geerling G, Dart JK. Management and outcome of cataract surgery in ocular cicatricial pemphigoid. Graefes Arch Clin Exp Ophthalmol. 2000;238(2):112-8.
- Miserocchi E1, Baltatzis S, Roque MR, et al. The effect of treatment and its related side effects in patients with severe ocular cicatricial pemphigoid. Ophthalmology. 2002;109(1):111-8.
- Kaushik P, Ghate K, Nourkeyhani H, et al. Pure ocular mucous membrane pemphigoid in a patient with axial spondyloarthritis (HLA-B27 positive). Rheumatology. 2013;52:2097-2099.
- Sotozono C, Inatomi T, Nakamura T, et al. Cultivated oral mucosal epithelial transplantation for persistent epithelial defect in severe ocular surface diseases with acute inflammatory activity. Acta Ophthalmologica. 2014;92(6):e447-e45.
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE

