CASE REPORT
DISEASE
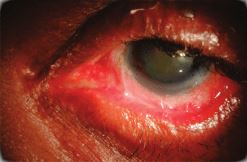
Ocular Cicatricial Pemphigoid (OCP) is considered a subtype of Mucous Membrane Pemphigoid, and these terms are sometimes used interchangeably.
Ocular Cicatricial Pemphigoid (OCP) is a type of autoimmune conjunctivitis that leads to cicatrization (i.e. scarring) of the conjunctiva. If OCP is left untreated, it can lead to blindness.
The exact pathogenesis of OCP remains to be elucidated but the existing evidence supports a Type II hypersensitivity response caused by an autoantibody to a cell surface antigen in the basement membrane of the conjunctival epithelium and other similar squamous epithelia.
Investigations into the underlying target antigen have led to several possible suspects. The autoantigens responsible for bullous pemphigoid (BP230 (i.e. Bullous pemphigoid antigen I, a desmoplakin) and BP180 (i.e. Bullous pemphigoid antigen II, a transmembrane hemidesmosome)) were studied, and the sera of patients with OCP was shown to bind these antigens.
However, further investigation supports that the more likely autoantigen is actually the beta-4 subunit of the alpha-6 beta-4 integrin of hemidesmosomes.
Studies of HLA (human leukocyte antigen) typing have found an increased susceptibility to the disease in patients with HLA-DR4.
The HLA-DQB1*0301 allele in particular shows a strong association with OCP and other forms of pemphigoid disease.
HLA-DQB1*0301 is thought to bind to the beta-4 subunit of the alpha-6 beta-4 integrin (the suspected autoantigen in OCP).
Incidence rates vary between 1 in 12,000 to 60,000. A study in the UK found that Ocular Cicatricial Pemphigoid (OCP) represents 61% of cicatricial conjunctivitis and is estimated to occur with an incidence of 1 in 1 million.
Women are affected more than men by a ratio of 2:1. Age on onset is usually age 60 to 80 and rarely younger than 30. There is no racial predilection.
Diagnosis
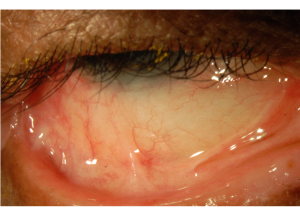
Diagnosis is based on clinical signs and positive direct immunofluorescence testing of the conjunctiva. Conjunctival biopsy of an actively involved area is needed and the conjunctival tissue must be submitted unfixed for analysis.

If involvement is diffuse, a biopsy of the inferior conjunctival fornix is recommended. A judicious biopsy is advisable as Ocular Cicatricial Pemphigoid (OCP) is an obliterating disease of the conjunctiva and only the minimal amount of tissue necessary should be removed.
Alternatively, a biopsy of an active oral mucosa lesion can be diagnostic as well. Immunofluorescence reveals linear staining of the epithelial basement membrane zone.
The sensitivity of immunofluorescence may be as low as 50%, especially for longstanding/severe cicatrization because of the loss of immunoreactants and the destruction of the basement membrane in longstanding disease.
Serological testing is not routinely used in diagnosis. Sequential photographs are useful to monitor clinical progression.
Differential Diagnosis
The differential diagnosis of Ocular Cicatricial Pemphigoid (OCP) is broad as it encompasses the differential for cicatricial conjunctivitis.
The differential includes infectious etiologies such as trachoma, inflammatory etiologies such as rosacea, autoimmune etiologies such as linear IgA disease, Graft Versus Host Disease (GVHD), and Stevens-Johnson Syndrome (SJS), allergic etiologies such as atopy, conjunctival trauma, chemical burns, medicaments, radiation, and neoplasia.
A common confounder of clinical diagnosis is medicamentosa, which results in a condition called pseudopemphigoid.
Pseudopemphigoid is clinically identical to OCP but is caused by the long-term use of certain offending topical medications.
Conjunctival biopsies may show linear staining of the conjunctival basement membrane zone. Differentiation from Ocular Cicatricial Pemphigoid (OCP) is difficult. Resolution with discontinuation of the offending agent is diagnostic.
Several topical medications have been implicated, including pilocarpine, epinephrine, timolol, idoxuridine, echothiophate iodide, and demecarium bromide.
MANAGEMENT
Without treatment, the disease progresses in up to 75% of patients. While systemic treatment stops the progression of cicatrization in most patients, it fails in approximately 10% of them.
Systemic therapy is necessary for Ocular Cicatricial Pemphigoid (OCP) as ocular involvement comprises a high-risk subset of MMP and is insufficiently treated with topical therapy alone.
Systemic treatment is best managed by a physician trained in the management of anti-inflammatory and immunomodulatory treatment given the significant risk of systemic complications necessitating frequent blood test monitoring.
Several drugs are effective in treating Ocular Cicatricial Pemphigoid (OCP) and a step-wise approach of escalation of therapy when there is insufficient response is recommended.
Topical therapy can be used as an adjunct for surface disease but should not be used in place of systemic therapy.
Topical therapy includes optimizing lubrication of the ocular surface with artificial tears and punctual plugging.
Topical and subconjunctival steroids can relieve symptoms but are ineffective for the treatment of the underlying disease.
Topical cyclosporine has been found to be ineffective while topical tacrolimus has been shown to be successful in small case series. Subconjunctival mitomycin-c has also been investigated in small case series with variable effects.
If the disease remains quiescent following a few years of systemic therapy, many practitioners are often able to discontinue systemic therapy successfully. However, it is important to continue to monitor the patient for recurrence of the disease as up to 22% of patients relapse.
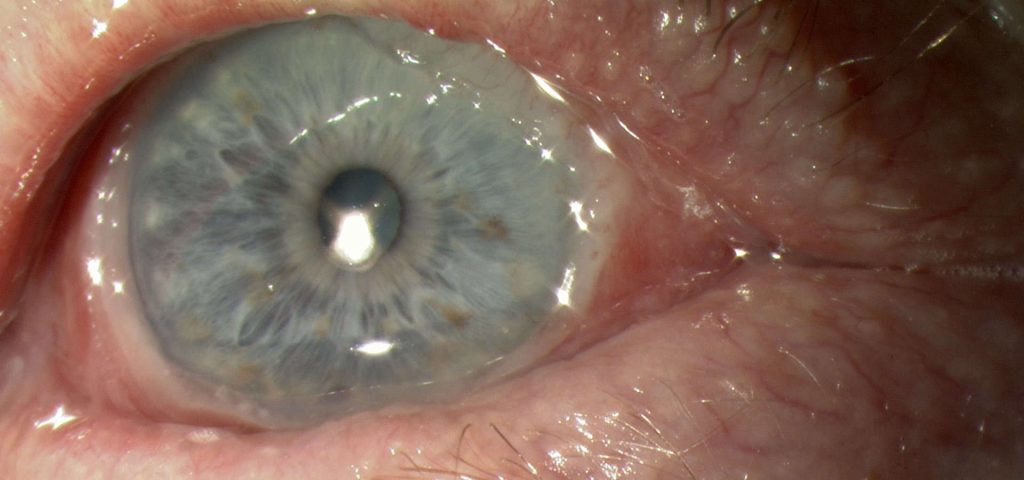
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Arafat SN, Suelves AM, Spurr-Michaud S, et al. Neutrophil Collagenase, Gelatinase and Myeloperoxidase in Tears of Stevens-Johnson Syndrome and Ocular Cicatricial Pemphigoid Patients. Ophthalmology. 2014;121(1):79-87.
- Ophthalmic Pathology and Intraocular Tumors. Basic and Clinical Science Course (BCSC). American Academy of Ophthalmology, 2014; pp54-56.
- External Disease and Cornea. Basic and Clinical Science Course (BCSC). American Academy of Ophthalmology, 2014; pp344-345.
- Tyagi S, Bhol K, Natarajan K, Livir-Rallatos C, Foster CS, Ahmed AR. Ocular cicatricial pemphigoid antigen: Partial sequence and biochemical characterization. Proc. Natl. Acad. Sci. 1996;93(25):14714-14719.
- Zakka LR, Reche P, Ahmed AR. Role of MHC Class II Genes in the pathogenesis of pemphigoid. Autoimmunity Reviews. 2011;(11):40–47.
- Bhol KC, Dans MJ, Simmons RK, et al. The autoantibodies to alpha 6 beta 4 integrin of patients affected by ocular cicatricial pemphigoid recognize predominantly epitopes within the large cytoplasmic domain of human beta 4. J Immunol. 2000 Sep 1;165(5):2824-9.
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE

