DISEASE
Arteritic Anterior Ischemic Optic Neuropathy (AAION) is an acute, often painful optic neuropathy that occurs predominantly in elderly patients over age 50 but with increasing incidence each decade thereafter and can cause permanent loss of vision. Ischemia occurs at the head of the optic nerve in relation to structural crowding of the nerve fibers, impairing perfusion and leading to optic disc edema.
There is thought to be a genetic component to the disease, as evidence shows Caucasians are affected at a higher rate, but it has been reported in many different races and ethnicities.
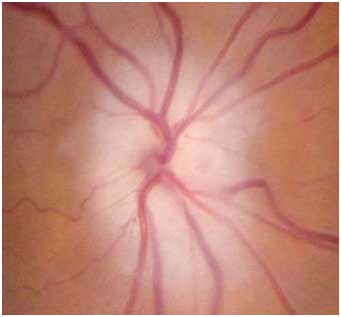
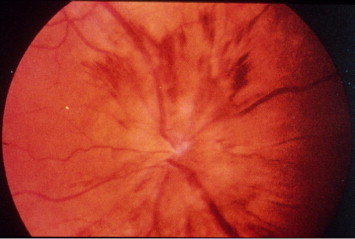
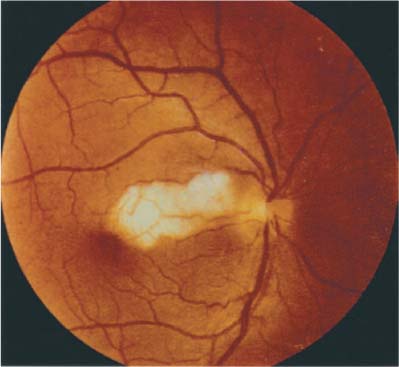
Patients on the exam can often show many different signs to lead to the right diagnosis. Some important signs on the exam include seeing the optic nerve swollen and pale (chalky color of the optic disc seen) upon ophthalmoscope, retinal cotton wool spots located at the posterior pole, and sometimes central retinal artery occlusion due to this artery and the SPCA both deriving from the ophthalmic artery.
Physical exam may also reveal diplopia, ptosis, nystagmus, or pain or nodularity upon palpitation of the temporal artery.
An elevated erythrocyte sedimentation rate (ESR) (up to 70-120mm/min) and/or serum C reactive protein (CRP) may aid in diagnosis.
A 97% specificity for temporal arteritis has been reported in cases of AAION in which both ESR and CRP were elevated.
Patients with NA-AION do not show these types of abnormalities. Other tests in GCA include: platelet count for possible thrombocytosis, leukocyte count, and hemoglobin levels.
Platelet count is often elevated acutely in cases of Arteritic Anterior Ischemic Optic Neuropathy (AAION) and can be used in conjunction with elevated ESR and CRP levels to make a preliminary diagnosis.
Confirmation of the diagnosis of temporal arteritis by superficial temporal artery biopsy is recommended in cases of AION with clinical suspicion of arteritis.
Positive biopsy findings (intimal thickening, internal limiting lamina fragmentation, and chronic inflammatory infiltrate with giant cells) are confirmatory for GCA.
A negative biopsy doesn’t rule out arteritis (both discontinuous arterial involvement (‘skip lesions’) and solely contralateral temporal artery inflammation may result in false-negative results) with recent reports showing a 3-5% false-negative error rate.
If an initial biopsy is found to be negative and suspicion for GCA is high, a biopsy of the contralateral temporal artery should be considered.
Magnetic Resonance Imaging has recently provided evidence that it may be able to distinguish between Arteritic Anterior Ischemic Optic Neuropathy (AAION) and NA-AION.
The imaging scores identified the acute stage of giant cell arteritis-related anterior ischemic neuropathy with a statistically significant relationship between the side of the AION and the side of the “central bright spot” i.e. optic nerve head enhancement.
Ultrasound(US) of the temporal artery can provide some insight as well. It reveals characteristic dark wall swelling (halo) and acute occlusions in active Arteritic Anterior Ischemic Optic Neuropathy (AAION).
The temporal artery duplex ultrasound has demonstrated a sensitivity and specificity of 87% and 96% respectively with regard to clinical diagnosis.
US provides a noninvasive technique that can be used after seeing a patient with elevated ESR, CRP, and platelet levels.
It remains to be proven if ultrasound will one day be able to obviate the temporal artery biopsy which remains the current gold standard.
MANAGEMENT
Steroids
Early steroid treatment is essential. High-dose systemic corticosteroids are standard. Intravenous methylprednisolone at 1g/day for the first three days has been recommended for severe cases but has not been subjected to a head-to-head trial against oral steroids in GCA.
Oral prednisone in the range of 60-100mg/day may be used initially and for follow-up to intravenous pulse therapy.
Treatment is usually continued at a high dose for several months before beginning taper but may be required for several years in severe cases to avoid permanent vision loss.
Tocilizumab is a monoclonal antibody humanized for the treatment of AAION. It works by binding to the alpha chain on the human interleukin 6 (IL-6) receptor.
Through binding, tocilizumab blocks signaling and downregulates the acute phase reactions. This monoclonal antibody has demonstrated effectiveness as a non-corticosteroid therapy for those dealing with Arteritic Anterior Ischemic Optic Neuropathy (AAION).
In some of the most recent literature, tocilizumab was very effective against corticosteroid-resistant AAION, causing symptoms to halt immediately upon the first dose.
However, more research into its ability to serve a protective role against bilateral blindness must be conducted to rule out any confounding variables. Tocilizumab received FDA approval in 2017 for the treatment of giant cell arteritis.
Other Treatment
Methotrexate is one of the most widely studied “steroid-sparing” agents. Also known as a chemotherapy agent, methotrexate has demonstrated some great benefits to those patients dealing with Arteritic Anterior Ischemic Optic Neuropathy (AAION).
A recent study indicated that the drug was able to significantly increase the probability of achieving a sustained discontinuation of using corticosteroids as well as decreasing the risks of relapses with the disease.
Corticosteroid therapy while effective, can be very toxic leading to almost 60% of individuals getting major side effects such as diabetes or cataracts.
At this time, methotrexate looks to serve best as a way to reduce exposure to corticosteroids and their adverse effects.
The best therapeutic option may be conjunction therapy, in order to decrease exposure and possible relapse for those patients with AAION.
Without treatment, visual loss occurs in 54-95% of GCA patients), typically within four months. With corticosteroid therapy, the rate of such decline is reduced to an estimated 13%.
Visual recovery of the affected eye that has treatment is poor with a 15-34% improvement rate, which is higher with intravenous therapy.
Worsening visual acuity has been reported in 9-17% despite therapy. Vision loss in both eyes is possible; however, most cases have indicated it to be frequent when one patient is unaware of vision loss in the first eye.

The incidence of having this bilateral involvement involves timing heavily as well as how aggressively corticosteroid therapy is utilized.
However, if left untreated, bilateral vision loss can proceed quickly from either optic nerve, retinal, or choroidal ischemia in up to 50% of cases.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Sohan Singh Hayreh, Ischemic optic neuropathy, In Progress in Retinal and Eye Research 2009; Volume 28, Issue 1, pp. 34-62,
- Arnold AC: Ischemic optic neuropathies. Ophthalmol Clin North Am 2001; 14: pp. 83-98
- Balducci, N., Morara, M., Veronese, C. et al. Graefes Arch., Optical Coherence Tomography, Clin Exp Ophthalmol, 2017; 255: 2255.
- Vionnet, Julien, et al. “Tocilizumab for giant cell arteritis with corticosteroid-resistant progressive anterior ischemic optic neuropathy.” Joint Bone Spine 2017.
- Beck RW, Servais GE, and Hayreh SS: Anterior ischemic optic neuropathy. IX. Cup-to-disc ratio and its role in pathogenesis. Ophthalmology 1987; 94: pp. 1503-1508
- Minagar, Alireza, et al. “Neurologic presentations of systemic vasculitides.” Neurologic clinics 28.1 2010: 171-184.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

