Vortex Vein Varix (VVV) DISEASE entity
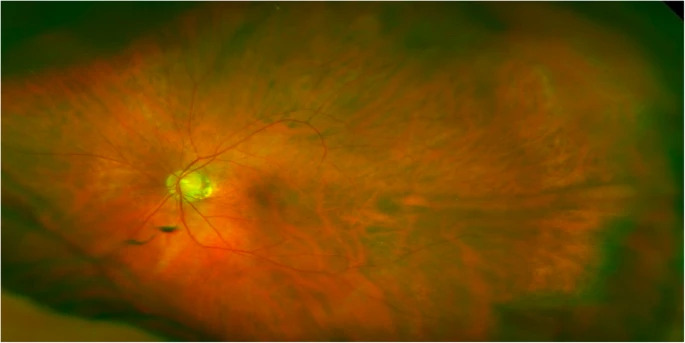
Vortex Vein Varicosis (VVV) are benign dilation of the vortex vein ampullae within the eye, presenting as unilateral or bilateral pouch-like structures at oblique meridians of the equator.
Although typically asymptomatic, they may lead to complications such as changes in the retinal pigment epithelium.
The etiology remains uncertain, with proposed mechanisms including kinking of the vortex vein, weaknesses in vessel walls, and fluctuations in intraocular pressure.
Diagnosis relies on clinical examination, with dynamic funduscopy being a key diagnostic tool. Imaging modalities such as OCT and ICGA provide confirmatory evidence.
Vortex vein varices are characterized by the dilation of vortex vein ampullae, benign elevations within the eye.
Typically, they manifest as single unilateral or multiple bilateral brownish-red to gray-colored pouches or teardrops located at oblique meridians of the equator.
While most varices range from 1 to 3 disc diameters in size, larger variants have been reported, with the larger ones potentially more prevalent in superior quadrants, particularly the supratemporal region.
The prevalence of physiologic vortex vein ampullae, which are present in about 44% of individuals, provides some context for understanding the occurrence of vortex vein varices.
However, the prevalence specifically of dilated vortex vein varices is less well documented, given their rare and often incidental nature.
Vortex vein varices may be incidentally discovered in patients referred for follow-up after experiencing symptoms of posterior vitreous detachment (PVD).
However, it is not believed that they are directly associated with floaters or photopsia. Although vortex vein varices generally do not cause symptoms, they can exert pressure on the underlying choriocapillaris, leading to changes in the retinal pigment epithelium (RPE).
Depending on the individual’s ocular background pathologies or surgical history, they may be associated with other signs or symptoms.
Clinically, distinguishing them from chorioretinal pathologies requiring treatment or follow-up, as well as more serious conditions like tumors, is crucial.

Digital compression or a 3-mirror examination can result in the diminished size or disappearance of varices. In cases where prompt diagnosis is challenging, further investigation with ultrasound B-scan, fluorescein angiography (FA)/indocyanine green angiography (ICG), or optical coherence tomography (OCT) scans may be necessary to confirm the diagnosis.
Factors such as weaknesses in the extracellular matrix and vessel walls, along with low intraocular pressure or high external pressure compromising vortex vein drainage, may contribute to their development.
Vortex Vein Varix (VVV) Diagnosis
Diagnosis of vortex vein varices typically involves clinical evaluation supported by imaging studies.
During a comprehensive eye examination, ophthalmologists may observe characteristic signs such as unilateral or bilateral brownish-red to gray-colored pouch or teardrop subretinal structures, often located at oblique meridians of the equator.
These elevations may range from 1 to 3 disc diameters in size, with larger variations reported.
Digital compression or examination with a 3-mirror lens may result in the reduction or disappearance of these elevations, which is a key feature for diagnosis.
This dynamic funduscopic finding, coupled with patient history and clinical presentation, provides valuable diagnostic information. Once the diagnosis is confirmed, further unnecessary investigations should be avoided.
However, in cases where clinical examination alone is inconclusive or further assessment is necessary, additional imaging modalities such as optical coherence tomography (OCT), indocyanine green angiography (ICGA), or ultrasound imaging may be utilized.
On spectral-domain OCT (SD-OCT), vortex vein varices typically appear as crescent-shaped elevations with larger choroidal veins merging towards the elevation.
These imaging findings help confirm the diagnosis and provide valuable information about the morphology and extent of the varices.

Overall, the combination of clinical evaluation, dynamic funduscopy, and imaging studies allows for accurate diagnosis and assessment of vortex vein varices, facilitating appropriate management and follow-up care.
MANAGEMENT of Vortex Vein Varix (VVV)
Management of Vortex Vein Varicosis (VVV) aims to alleviate symptoms, prevent complications, and address underlying causes when possible.
General treatment:
No specific treatment: Generally, no specific treatment is available for Vortex Vein Varicosis (VVV) itself.
Management of associated conditions: Any associated or background diseases should be treated accordingly.
For example, if there are underlying conditions such as high myopia or other ocular pathologies like scleritis, these may require specific management.
Medical therapy:
Medical therapy for vortex vein varicosis may involve medications to reduce choroidal congestion, control intraocular pressure, or manage associated systemic vascular diseases.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Weidmayer SL, Demirci H. The spontaneous resolution of a vortex vein varix: case report. BMC Ophthalmol. 2021 Feb 24;21(1):101. doi: 10.1186/s12886-021-01861-2. PMID: 33627084; PMCID: PMC7903696
- Shields JA, Shields CL. Non-neoplastic conditions that can simulate posterior uveal melanoma and other intraocular neoplasms. In: Shields JA, Shields CL, eds. Intraocular Tumors: An Atlas and Textbook. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008:177-195.
- Shields JA, Mashayekhi A, Ra S, Shields CL. Pseudomelanomas of the posterior uveal tract: The 2006 Taylor R. Smith lecture. Retina. 2005;25(6):767-771.
- Gunduz K, Shields CL, Shields JA. Varix of the vortex vein ampulla simulating choroidal melanoma: report of four cases. Retina. 1998;18(4):343-347.
- Osher RH, Abrams GW, Yarian D, Armao D. Varix of the vortex ampulla. Am J Ophthalmol. 1981;92(5):653-660.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

