DISEASE
Lens-induced uveitis (LIU) is an uncommon autoinflammatory condition where the immune system’s natural tolerance of lens protein is abandoned, most often occurring after traumatic or surgical lens injury.
This disease is also known by other names including Phacoanaphylactic endophthalmitis, phacogenic uveitis, and phacotoxic uveitis.
It was first described in medical literature in 1919 and termed “endophthalmitis anaphylactica” in a 1922 case series of patients who developed non-infectious endophthalmitis days to weeks following extracapsular cataract surgery.
Contrary to what is suggested by such a name, this disease does not involve true anaphylaxis and does not feature an IgE-mediated response.
Lens-induced uveitis (LIU) remains a small fraction of clinically encountered cases of uveitis, especially with modern surgical techniques that include complete removal of the lens during cataract removal.
LIU is thought to be the result of an abnormal immune tolerance to lens proteins, resulting in a cell-mediated autoimmune phenomenon.
Researchers have argued against the mechanism of immune privilege and rejection of newly encountered self-antigens, noting the rare frequency of this condition despite the presence of extracapsular lens protein in asymptomatic individuals.
Instead, this condition is proposed to be caused by an abnormal recognition of self-antigens on lens material.
Diagnosis
History:
Evaluation for Lens-induced uveitis (LIU) should include a history with attention to recent ocular trauma or surgery on the affected eye.
While this condition is associated with a variable presentation in both latency and severity of symptoms, clinical symptoms typically emerge within two weeks of lens injury.

Symptoms:
Symptoms of Lens-induced uveitis (LIU) are limited to the traumatized eye while the contralateral eye is spared.
Symptoms typically include decreased vision, photophobia, conjunctival injection, and pain. The onset of symptoms may range from gradual to acute.
Signs:
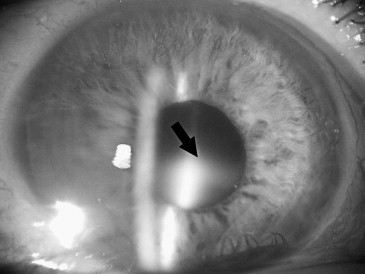
Slit-lamp examination of a patient with LIU may reveal lens fragments in the anterior chamber, corneal edema, anterior chamber cell and flare, keratic precipitates, and hypopyon.
There may or may not be a disturbance in visual acuity or intraocular pressure, given the highly variable presentation of this disease.

Diagnostic procedures:
Although Lens-induced uveitis (LIU) can be diagnosed clinically based on a careful history and slit-lamp examination, in practice, most cases require one or more diagnostic tests to be certain of the diagnosis.
Scanning electron microscopy or anterior segment optical coherence tomography (OCT) may be useful for detailed examination of the lens capsule, with evidence of capsular trauma supporting the diagnosis.
Confirmation of this disease may be achieved through needle biopsy with histopathology or cytology of the aqueous humor.
Cytological examination may discover evidence of the characteristic granulomatous response including macrophages and polymorphonuclear cells surrounding lens material, which is strongly suggestive of lens-induced uveitis.
MANAGEMENT
General Treatment:
The initial treatment strategy for lens-induced uveitis involves prompt screening for associated increased intraocular pressure by tonometry and initiation of aqueous suppressant therapy as needed.
Definitive management of this condition involves removing the offending lens material.
Medical Therapy:
Medical therapy in the preoperative period should aim to control intraocular pressure. This can be achieved with aqueous suppressants or systemic medications such as acetazolamide or mannitol if needed.
Topical or systemic steroids may have a role in the treatment of LIU depending on the severity of clinical presentation.
Preoperative antibiotic therapy is also recommended in Lens-induced uveitis (LIU) and may be used in cases where cataract extraction was previously performed as well as in those cases where the presumed cause of LIU is a hypermature cataract.
Surgery:
Surgical management is the definitive treatment for lens-induced uveitis. This is considered an emergency condition for which surgery should be performed following the reduction of IOP to the physiologic range if it is elevated.
The surgical approach for LIU is tailored to the causative agent for clinical symptoms. In cases where there is a cataract present in the affected eye, cataract extraction is recommended.

The technique of cataract removal, whether via lens aspiration, phacoemulsification, manual small incision cataract surgery, or extracapsular cataract extraction, should depend on patient characteristics as well as surgeon preference.
For patients with a history of cataract removal, washout of retained lens fragments is preferred. Washing of the anterior chamber is performed in cases where the posterior lens capsule is intact.
If the posterior capsule has been violated and lens fragments have descended to the vitreous, pars plana vitrectomy is indicated.
Cases of lens-induced uveitis following non-cataract surgery have also been described in the literature. These include, for example, lens-induced uveitis with the onset of symptoms days following a pars plana vitrectomy complicated by injury to the posterior lens capsule during gas injection.
In such cases, where lens material was displaced into the vitreous cavity, repeat pars plana vitrectomy with removal of offending lens material has resulted in favorable outcomes.
In severe cases without the removal of lens fragments, severe pain, and blindness in the affected eye may develop as early as one year after lens trauma.
Such cases have previously been effectively treated with enucleation of the eye and insertion of an orbital implant.
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Nche EN, Amer R. Lens-induced uveitis: an update. Graefes Arch Clin Exp Ophthalmol. 2020;258(7):1359-1365. doi:10.1007/s00417-019-04598-3
- Thach AB, Marak GE, McLean IW, Green WR. Phacoanaphylactic endophthalmitis: a clinicopathologic review. Int Ophthalmol. 1991;15(4):271-279. doi:10.1007/BF00171031
- Chung, Hum, Choi, Dong-Gyu. Clinical analysis of uveitis.
- McMahon MS, Weiss JS, Riedel KG, Albert DM. Clinically unsuspected phaco anaphylaxis after extracapsular cataract extraction with intraocular lens implantation. Br J Ophthalmol. 1985;69(11):836-840. doi:10.1136/bjo.69.11.836
- Rajesh B, Hussain R, Gopalakrishnan M, Giridhar A. Phacoantigenic Reaction Masquerading as Postoperative Endophthalmitis in a Silicone Oil-filled Eye. Middle East Afr J Ophthalmol. 2016;23(4):318-320. doi:10.4103/0974-9233.194088
- Sridhar U, Tripathy K. Lens Induced Inflammation. In: StatPearls. StatPearls Publishing; 2022. Accessed February 8, 2022.
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE

