Retinal Angiomatous Proliferation (RAP) DISEASE entity
Retinal Angiomatous Proliferation (RAP) is a neovascularization that starts at the retina and progresses posteriorly into sub-retinal space; eventually, the neovascularization reaches the choroidal circulation and forms retinal-choroidal anastomoses.

This is distinct from choroidal neovascularization (CNV) in AMD which originates from the choroid and can erode through the retinal pigment epithelium and communicate with the retinal circulation through a different mechanism, resulting in a chorioretinal anastomosis.
There has been some controversy on whether neovascularization arises from the retina or from the choroid. Yannuzzi et al stated in their last review that it is possible that angiogenesis starts in the retina, choroid, or both, and they proposed an alternative name for this process: Type 3 neovascularization.
This new designation would apply to neovessels within the retina and right underneath and it integrates with the classical neovascularization classification by Gass (Type 1 neovessels being located under the retinal pigment epithelium and Type 2 under the neurosensory retina). Retinal Angiomatous Proliferation (RAP) remains however the most widely used denomination.
Several series have studied the prevalence of RAP, with estimates ranging from 10 to 21% of exudative AMD. In the Comparison of Age-Related Macular Degeneration treatment trials (CATT), the prevalence of RAP was 10.7%.
Patients with RAP tend to be older than patients with other forms of neovascular AMD (mean age of 79 vs 76, respectively).
It is most common in white patients, and may also be seen in Asian patients. As of 2008, according to Yannuzzi and colleagues, there was no report of RAP in black patients.
Diagnosis
Clinical diagnosis:
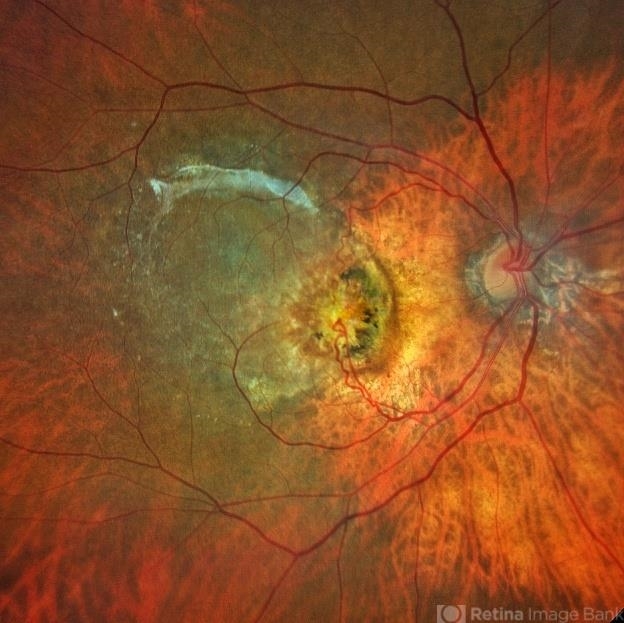
The initial lesion is located extrafoveally, presumably because of a lack of capillaries in the foveal avascular zone.
The presence of small macular hemorrhages, sometimes punctiform, often multiple, associated with edema in an eye with soft drusen, is highly suggestive of Retinal Angiomatous Proliferation (RAP) in its initial stages.
Hemorrhages can be pre-, intra, or subretinal. Large subretinal hemorrhage is rarely seen in stages I and II. As angiogenesis progresses, tortuous, dilated retinal vessels, sometimes showing retino-retinal anastomoses can be found.
Involvement is typically bilateral, with 80% of fellow eyes affected after 1 year and 100% before 3 years.
- older patients in RAP
- intraretinal changes – hemorrhage, exudate, and fluid more common
- large subretinal bleed rare
- preretinal hemorrhage can be seen
- usually not at the fovea
- In all cases of pigment epithelial detachment after 50 years of age -polypoidal choroidal vasculopathy (PCV) and RAP need to be excluded with ICG angiogram preferably digital, scanning laser ophthalmoscope based system (eg., Spectralis, Heidelberg Engineering).
Diagnostic procedures
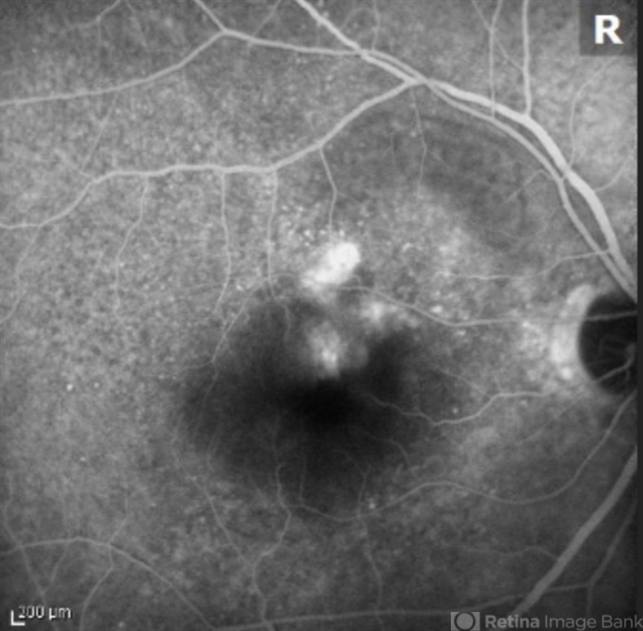
Fluorescein angiography (FA):
Fluorescein angiography can help in the diagnosis of early-stage Retinal Angiomatous Proliferation (RAP) lesions, but in later stages, the dye stains the whole vascular-exudation complex and can be confused with occult CNV.
- Features on FA:
- Required: Focal area of intense intraretinal hyperfluorescence (hot spot) in the early phase of FA
- + 1 or more of the following signs:
- Focal intraretinal superficial hemorrhages
- lipid
- serous or fibrovascular pigment epithelial detachments
- retinal vascular abnormalities, such as anastomoses between retinal vessels, anastomoses between retinal and choroidal vessels, or anastomoses between retinal vessels and the underlying CNV complex.
Indocyanine green angiography (ICG)
- Shows hot spot in mid and/or late frames
- hairpin loop (linked perfusing retinal arteriole and draining retinal venule)
- Retinal Angiomatous Proliferation (RAP) shows typically late-phase leakage of the ICG molecule into intraretinal spaces or cystoid edema. The ICG molecule has an affinity for fibrin, which is present in the cystic spaces.
- ICG can also reveal the retinochoroidal anastomosis.
Optical coherence tomography (OCT)
- OCT is useful in the initial stage of RAP to image the vessels and the cystic spaces within the retina. As the disease progresses and a serous or vascularized PED occurs, changes beneath the pigment epithelium become difficult to assess accurately. Sub–pigment epithelium blood, exudates, and neovascularization produce photo reflectance that can be indistinguishable.
- New angio-OCT systems have the potential to become a very useful diagnostic tool for this disease.
Differential diagnosis
- Idiopathic parafoveal telangiectasia is a condition involving dilation of retinal capillaries located near the fovea, in one or both eyes. Telangiectasias are not associated with serous PED, the RPE is healthier, and choroidal neovascularization associated with parafoveal telangiectasias occurs less frequently.
- Other forms of choroidal neovascularization (CNV) include polypoidal choroidal vasculopathy (PCV). Retinal hemorrhages in PCV are normally larger, with round reddish-orange macular lesions being observed in the eye fundus. Polyps can be seen in OCT as abrupt protrusions from the REP/Bruch’s membrane band, often associated with neurosensory detachment.
- macular branch retinal venous occlusion
MANAGEMENT
Medical therapy:
Retinal Angiomatous Proliferation (RAP) demonstrates a good response to anti-vascular endothelial growth factor agents (Anti-VEGF).

In the Comparison of Age-Related Macular Degeneration treatment trials (CATT), when treated with intravitreal ranibizumab or bevacizumab, eyes with RAP were less likely to have fluid, FA leakage, scar, and subretinal hyperreflective material were compared with all other eyes with neovascular AMD but without RAP.
Visual acuity outcomes at 1 year were better in the RAP group than in the non-RAP group, however, these differences did not persist at year 2.
In addition, eyes with RAP were also found to be more likely to have geographic atrophy than eyes without RAP.
Other therapies include
- laser photocoagulation of feeder vessels
- Intravitreal triamcinolone to reduce exudation (intraretinal/subretinal) followed 10 days later by PDT.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Daniel, E., Shaffer, J., Ying, G.-shuang, Grunwald, J. E., Martin, D. F., Jaffe, G. J., & Maguire, M. G. (2016). Outcomes in eyes with retinal angiomatous proliferation in the comparison of age-related macular degeneration treatments trials (CATT). Ophthalmology, 123(3), 609–616. https://doi.org/10.1016/j.ophtha.2015.10.034
- Yannuzzi LA, Freund KB, Takahashi BS. Review of retinal angiomatous proliferation or type 3 neovascularization. Retina. 2008 Mar;28(3):375-84. doi: 10.1097/IAE.0b013e3181619c55. Review. PubMed PMID: 18327130.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

