CASE REPORT
A 55-year-old male presented to an ophthalmology clinic with blurred vision in his left eye over the past two weeks.
He has a history of type 2 diabetes mellitus diagnosed 10 years ago, managed with oral hypoglycemic agents and diet control, denying ocular trauma or recent illness.
On examination, his visual acuity was 20/20 in the right eye and 20/40 in the left eye, with normal intraocular pressure bilaterally.
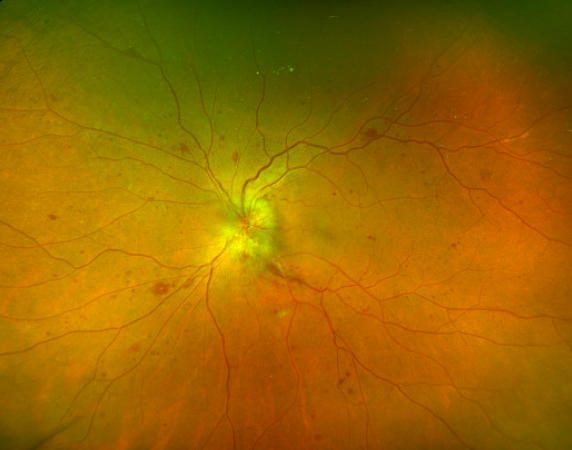
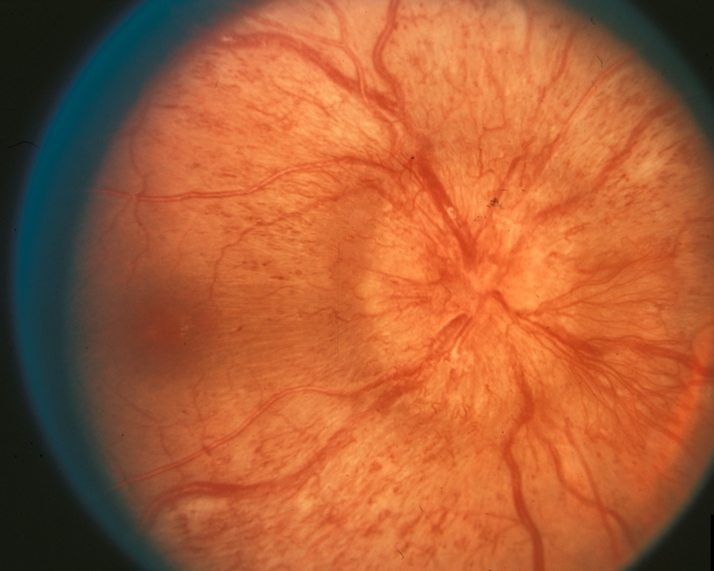
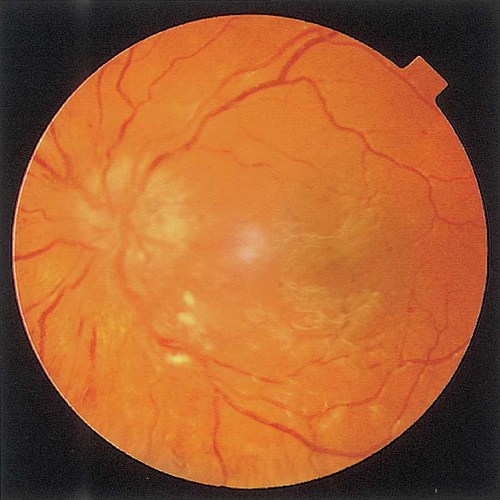
Anterior segment examination was unremarkable. Fundus examination of the left eye revealed optic disc swelling with blurred margins and mild hemorrhages along the disc margin, with no other abnormalities noted.
Further investigations confirmed diabetic Papillopathy and ruled out other causes of optic disc edema:
- Optical Coherence Tomography (OCT) showed peripapillary retinal nerve fiber layer thickening and mild macular edema in the left eye.
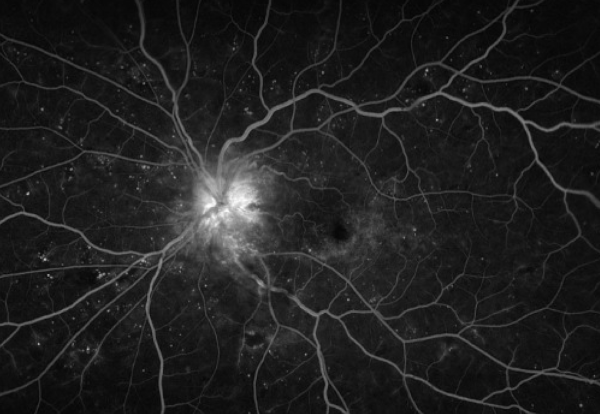
- Fundus Fluorescein Angiography (FFA) demonstrated hyperfluorescence around the optic disc, consistent with leakage from dilated peripapillary capillaries.
- Blood tests revealed an elevated HbA1c level of 9.2%, indicating poor glycemic control.
Based on the clinical findings and investigations, the patient was diagnosed with diabetic papillopathy in the left eye.
Diabetic papillopathy DISEASE entity
Diabetic papillopathy or diabetic papillitis is a relatively rare ocular manifestation of diabetes mellitus. Diabetic papillopathy was first described in a series of teenage, type 1 diabetic patients in 1971 by Lubow and Makley, but since that time, it has been reported in both type 1 and type 2 diabetic patients of all ages.
It is most often unilateral, however, bilateral cases may occur. Patients may report blurred vision, but many present with no symptoms.
Diabetic papillopathy causes optic disc edema with minimal visual changes, which distinguishes it from other optic neuropathies.
Diabetic papillopathy remains a controversial topic as some authors believe that it is a form of non-arteritic anterior ischemic optic neuropathy (NAION) but this has yet to be determined.
This is a disease of the optic nerve typically associated with diabetes mellitus, possibly further exacerbated in patients who have had rapid correction of their blood glucose levels.
Diabetic papillopathy Symptoms
Patients with diabetic papillopathy tend to be asymptomatic but may present with mild blurring of vision.
Interestingly, signs of optic neuropathy such as a relative afferent pupillary defect (RAPD), dyschromatopsia, and visual field defects are typically not seen.
Diagnostic procedures
Optical Coherence Tomography (OCT)
OCT of the optic nerve typically shows the increased thickness of the papillary profile without loss of the retinal nerve fiber layer (RNFL).
OCT macula can often be unremarkable, though edema from the nerve may track towards the macula.
Fluorescein angiography (FA)
FA is useful in distinguishing diabetic papillopathy from other etiologies, such as neovascularizing the disc (NVD) and NAION. Diabetic papillopathy may present with prominent disc telangiectasias and associated disc edema, which can be easily confused for NVD.
However, diabetic Papillopathy usually demonstrates disc and peripapillary leakage with the radial distribution of fluorescein in dilated vessels versus the random pattern of vasculature with intravitreal leakage in NVD.
In cases without prominent telangiectasia, the delayed filling pattern of the disc can mimic that seen in NAION. In this case, it is important to correlate with optic nerve dysfunction, which would be seen in NAION rather than diabetic papillopathy.
Diabetic papillopathy MANAGEMENT
General treatment
There are no well-studied treatments for diabetic papillopathy. Although it is not proven that diabetic microangiopathy is the etiology of disc edema, a few studies looked at the effectiveness of different treatment modalities based on this theory.
Observation is a reasonable initial approach as these patients can improve without intervention (assuming life-threatening causes for disc edema have been excluded).
Corticosteroids
There are a few studies that reported the favorable outcomes of a periocular steroid injection (including subtenon triamcinolone) in diabetic papillopathy.
An observational study by Mansour et al. looked at 5 diabetic patients who received periocular steroid treatment for severe symptomatic diabetic papillopathy.
This study found that the duration of diabetic papillopathy was shortened from a median of 5 months to 3 weeks and rapid visual recovery was seen.
Another study looked at the effect of oral corticosteroids in preventing the progression of diabetic papillopathy to NAION.
An observational cohort study done by Hayreh et al. showed that there is no significant difference in the incidence of progression between patients who received steroid treatment and patients who did not.
Intravitreal anti-vascular endothelial growth factor (Anti-VEGF) agents
Several case reports described the use of intravitreal anti-VEGF with improvement in vision, however, no prospective studies have been undertaken to see if this varies the course of the disease. Larger clinical studies are needed to prove the efficacy and safety of anti-VEGF agents.
Prognosis
Diabetic papillopathy is generally known to have a good visual prognosis.
One study reported that approximately 92% of eyes had no changes in visual acuity after disc swelling resolved and 75% of the eyes had visual acuity better than 20/40 at the last visit.
In this study, optic disc edema spontaneously resolved in roughly 4-9 months.
However, there are some reported cases of vision loss in diabetic papillopathy possibly due to worsening diabetic retinopathy, development of disc neovascularization, or progression to NAION. In one study, 36% of the eyes progressed to NAION with a mean duration of 16.8 weeks.
Although diabetic papillopathy is known to run a benign course, regular testing should be done to evaluate for changes and the possibility of progression.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Lubow M, Makley TA Jr. Pseudopapilledema of juvenile diabetes mellitus. Arch Ophthalmol 1971;85:417–422.
- Bayraktar Z, Alacali N, Bayraktar S. Diabetic papillopathy in type II diabetic patients. Retina 2002; 22:752.
- Appen RE, Chandra SR, Klein R, Myers FL. Diabetic papillopathy. Am J Ophthalmol 1980;90:203–209.
- Pavan PR, Aiello LM, Wafai MZ, Briones JC, Sebestyen JG,Bradburry MJ. Optic disc edema in juvenile-onset diabetes.Arch Ophthalmol 1980;98:2193–2195.
- Barr CC, Glaser JS, Blankenship G: Acute disc swelling in juvenile diabetes. Clinical profile and natural history of 12 cases. Arch Ophthalmol 98: 2185–92, 1980
- Beri M, Klugman MR, Kohler JA, Hayreh SS. Anterior ischemic optic neuropathy. VII. Incidence of bilaterality and various influencing factors. Ophthalmology. 1987 Aug;94(8):1020-8.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

