CASE REPORT
A 34-year-old man was in good health until he failed to hit a ping-pong ball accurately one morning. Blackish dots appeared in the nasal upper visual field, and flashes blocked the vision in front of his left eye.
He was myopic with −11.0 diopter (D) in the right eye (OD) and −15.0 in the left eye (OS), and he underwent LASIK surgery seven years ago.
He visited our emergency department, where visual acuity (VA) revealed 20/20 (OD) and 20/32 (OS). No cells were noted at the anterior chamber (AC) or vitreous. His fundus seemed normal under dilated fundoscopy.
On the next day, vision decreased significantly to 20/25 (OD) and 20/63 (OS). Visual field (VF) examinations demonstrated bilateral enlarged blind spots and altitudinal defects.
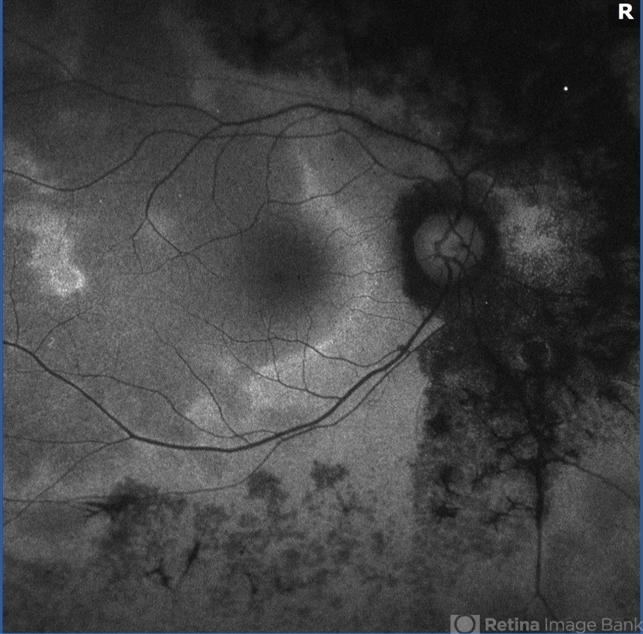
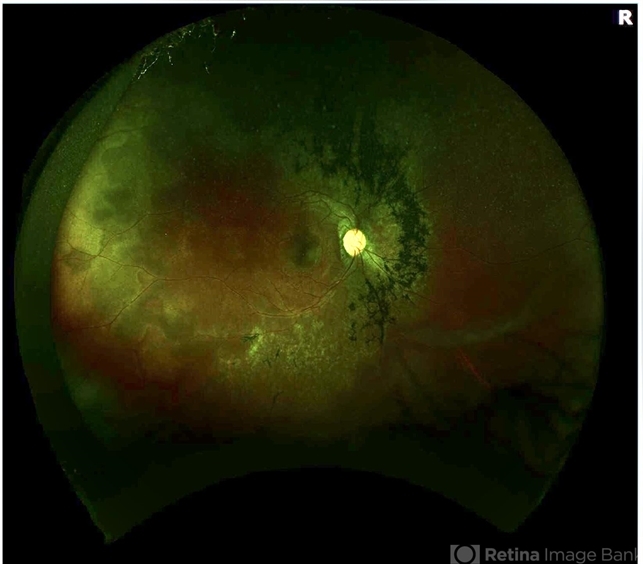
FA showed hyperfluorescence (OS) and inflammation of retinal small vessels. OCT examinations revealed parafoveal loss of the photoreceptor IS/OS junction.
ERG revealed decreased amplitude of the b wave in both eyes. According to his symptoms and examinations, Acute Zonal Occult Outer Retinopathy (AZOOR) was diagnosed.
Acute Zonal Occult Outer Retinopathy (AZOOR) DISEASE entity
Acute Zonal Occult Outer Retinopathy (AZOOR) was first described by Donald Gass in 1992; reporting on 13 cases presenting with acute vision loss/visual field defects with photopsias.
These patients had an acute loss of one or more large zones of outer retinal function with minimal fundus changes at presentation, with some patients having the involvement of the blind spot.
They demonstrated electroretinographic abnormalities, permanent visual field loss, and delayed development of clinically visible atrophic changes in the retinal pigment epithelium (RPE).
Acute Zonal Occult Outer Retinopathy (AZOOR) has been theorized to be associated with acute idiopathic blind-spot enlargement syndrome (AIBES), multiple evanescent white dot syndrome (MEWDS), acute macular neuroretinopathy (AMN) and other white dot syndromes, as symptoms and findings can overlap; however, this has yet to be clearly determined.
The majority of patients are young females in their mid-thirties and women have comprised approximately three-quarters of Acute Zonal Occult Outer Retinopathy (AZOOR) cases.
AZOOR has been observed in Caucasian patients predominantly; however, the disease has been seen in all ethnic groups. Myopia has been a reported association.
Acute Zonal Occult Outer Retinopathy (AZOOR) Diagnosis
Symptoms:
Patients often note sudden awareness of a scotoma, related to the zone of outer retinal dysfunction, alongside the presence of photopsia (described as “scintillating” or “shimmering” lights).
Visual acuity may be decreased. Some patients may report a viral infection preceding the symptoms.
The disease may progress to involve the second eye. A report of 51 patients followed for a median of 8 years demonstrated that 61% had unilateral involvement at onset, but 76% progressed to bilateral involvement by the final examination. The involvement was delayed by a mean of 50 months.
Signs:
Visual acuity is usually minimally affected early in the disease. The anterior chamber is quiet. Vitreous cells may be present but are usually minimal.
The fundus initially appears normal followed by retinal atrophy and mottling/mild pigmentary changes of the RPE in the areas involved as the disease progresses. The arterioles may become attenuated.
Acute Zonal Occult Outer Retinopathy (AZOOR) MANAGEMENT
Medical therapy:
No proven treatment exists. Systemic corticosteroids, immunosuppressive drugs (cyclophosphamide, methotrexate, azathioprine, etc.), antiviral (acyclovir and valacyclovir), and antibacterial (sulfadiazine and trimethoprim) medications have been tried with no consensus on the success. Spontaneous remission has also been observed.

Indeterminate improvements in vision and ophthalmic imaging/testing have been reported following varying regimes of intravenous and oral corticosteroids with tapering regimes but larger studies with control groups are needed.
In a study by Barnes et al, 9 eyes were treated with intravitreal steroid injections or implants and observed stable or improved vision.
There are cases reported of disease reactivation following prednisone tapers requiring steroid-sparing immunosuppressant therapy.
Prognosis
Due to the rarity of Acute Zonal Occult Outer Retinopathy (AZOOR), it is difficult to characterize the progression and prognosis of this disease and the clinical course can be variable.
Visual field defects tend to be permanent. Stabilization has been reported to have occurred within 6 months in the majority of patients (77-90%) after the initial progressive decline early in the disease.
Saito et al. also found in their study of 32 Japanese patients that the visual field parameters stabilized at 6 months, with only 2.6% continuing to worsen at the final visit (median of 31 months).

However, there is significant variability in the literature. Hoang et al report a case of a 55-year-old female patient followed up for thirteen years who despite treatment attempts with acyclovir and immunomodulatory drugs (periocular and systemic steroids, and cyclosporine) demonstrated no change in the progression with severe visual field constriction secondary to diffuse chorioretinal atrophy.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Gass JD. Acute zonal occult outer retinopathy. Donders Lecture: The Netherlands Ophthalmological Society, Maastricht, Holland, June 19, 1992. J Clin Neuroophthalmol. 1993;13:79-97
- Ryan, Stephen. Retina. 5th Ed. China: El Sevier Saunders, 2013:1368-1371
- Fletcher WA, Imes RK. Acute Idiopathic Blind Spot Enlargement and Acute Zonal Occult Outer Retinopathy: Potential Mimics of Neuro-Ophthalmic Disease. J Neuroophthalmol. 2020 Sep;40 Suppl 1:S43-S50
- Monson D, Smith J. Acute Zonal Occult Outer Retinopathy. Surv Ophthalmol 2011;56:23-35
- Gass JD, Agarwal A, Scott I. Acute Zonal Occult Outer Retinopathy: A Long-term Follow-up Study. Am J Ophthalmol 2002;134:329-339
- Gass JD. Are acute zonal occult outer retinopathy and the white spot syndromes (AZOOR complex) specific autoimmune diseases? Am J Ophthalmol 2003;135:380-381.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE


Thank you for your post. I really enjoyed reading it, especially because it addressed my issue. It helped me a lot and I hope it will also help others.
Thank you for writing this post. I like the subject too.