CASE REPORT
A 58-year-old male with a 10-year history of human immunodeficiency virus (HIV) infection, under consistent antiretroviral therapy (ART) with a CD4 count ranging between 50-100 cells/mm³ over the past 5 years, presented to an ophthalmology clinic with a two-week history of progressive vision loss in the left eye, described as a “curtain” descending over his vision, accompanied by floaters and flashes of light.
Clinical examination revealed visual acuity of 20/20 in the right eye and counting fingers at 1 meter in the left eye, with normal intraocular pressures and anterior segment examination bilaterally.
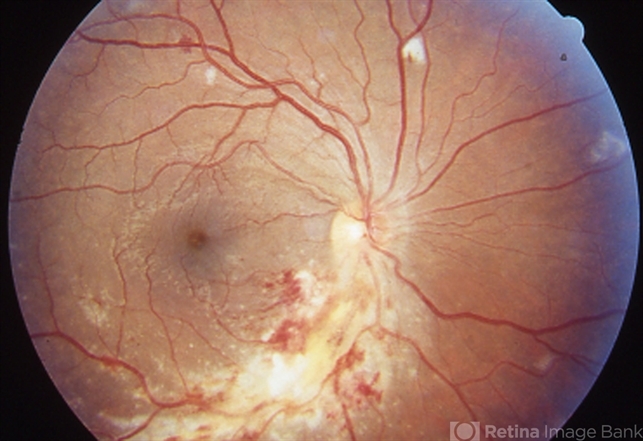
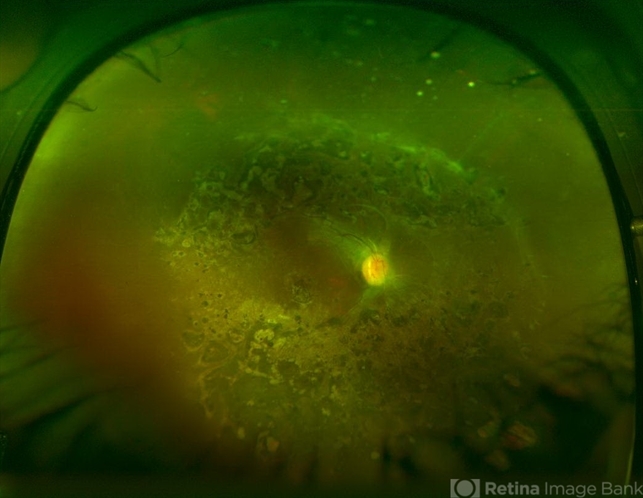
Posterior segment examination demonstrated creamy white retinal lesions with hemorrhagic borders extending from the peripheral retina to the posterior pole in the left eye, along with areas of retinal hemorrhage and detachment.
Fundus fluorescein angiography showed late-phase hyperfluorescence corresponding to the retinal lesions, optical coherence tomography revealed marked thickening of the retina with hyper-reflective areas, and CMV polymerase chain reaction (PCR) from aqueous humor was positive for CMV DNA, leading to a diagnosis of CMV retinitis in the left eye due to the patient’s immunocompromised status from HIV infection.
DISEASE
Cytomegalovirus (CMV) Retinitis is an acquired immunodeficiency syndrome (AIDS)-related opportunistic infection that can lead to blindness.
CMV retinitis occurred with higher frequency prior to the advent of antiretroviral therapy but has since been decreasing in well-developed countries, although still remains a prevalent condition in developing countries.
It is a viral retinitis that can also be seen in patients who are immunosuppressed for other reasons aside from AIDS. It is a full-thickness retinal infection that can lead to necrosis and retinal breaks and detachments.
CMV retinitis is caused by cytomegalovirus, a double-stranded DNA virus in the herpes viridae family. It is often associated with HIV/AIDS and was extremely rare prior to the AIDS epidemic.
It is also associated with severe immunosuppression from chemotherapy and autoimmune conditions requiring immunomodulators. With the advent of antiretroviral therapies, the incidence of CMV retinitis has decreased by 90% in the AIDS population.
Risk factors include HIV, CD4 count less than 50, or severe systemic immunosuppression. Recent reports have also demonstrated that local ocular immunosuppression can be a risk factor for CMV Retinitis.
There have also been case reports of CMV retinitis in the absence of immunosuppression.
Diagnosis
Diagnosis is largely clinical based upon the classic retinal findings and an immunosuppressive condition such as HIV; however, polymerase chain reaction (PCR) analysis of the vitreous or aqueous can further support the diagnosis. Differentiation from acute retinal necrosis/ARN is vital as treatment is different.
History
Patients present with decreased visual acuity and floaters. Some may present with flashing lights (photopsias) or blind spots (scotomata). One study showed 54% were asymptomatic.
Physical examination
Physical exam shows yellow-white retinal lesions that often start in the periphery and follow the vasculature centripetally.
However, it can start in the posterior segment. The classic findings are retinal hemorrhages with a whitish, granular appearance to the retina.
Each lesion has the most activity in the borders. Vitreous signs of inflammation may be minimal as most patients are severely immunosuppressed.
Very early CMV may resemble cotton wool spots, but with lesions larger than 750 µm, CMV must be considered. Three typical patterns have been described: a granular pattern, a fulminant/hemorrhagic appearance, or “frosted branch” angiitis.
Rhegmatogenous retinal detachment occurs in approximately one-third of patients when greater than 25% of the retina is involved. The presence of concurrent keratic precipitates in a stellate fashion can also suggest CMV uveitis.
Signs:
CMV retinitis can present as:
1. Fulminant – hemorrhagic necrosis on white/yellow cloudy retinal lesions. They may be centered around vasculature.
2. Granular – Found more often in the retinal periphery with little to no necrosis and hemorrhage.
3. Perivascular – The classic “frosted branch” angiitis shows white lesions surrounding the retinal vessels.
Symptoms:
Most patients are asymptomatic but may have floaters, flashes (photopsias), and blind spots (scotomata). Pain and photophobia are uncommon.
Clinical diagnosis:
The clinical diagnosis is made on history and classic retinal findings
Diagnostic procedures:
Diagnostic procedures can include aqueous or vitreous tap to test for CMV and other herpes viruses.

Laboratory test
In cases of unknown retinitis, aqueous or vitreous tap and PCR analysis for CMV can be done. Serologic antibodies for CMV are not helpful in the diagnosis of CMV retinitis– a positive CMV antibody titer reflects prior exposure.
Still, it does not diagnose the retinitis specifically, and a negative CMV antibody titer does not eliminate the chance of CMV retinitis, as immunosuppressed patients may not mount appropriate titers.
Differential diagnosis
Early CMV can resemble cotton wool spots. It may be confused with HIV retinopathy, which is actually more common the CMV retinitis.
HIV retinopathy occurs in 50-70% of patients and is characterized by intraretinal hemorrhages, cotton wool spots, and microaneurysms.
For small lesions that are hard to differentiate from cotton wool spots, serial exams should be performed, which will show enlargement of the CMV lesions.
Immunosuppression should be treated like a spectrum; some patients are more immunosuppressed than other individuals.
For cases of minor immunosuppression, CMV retinitis may present as acute retinal necrosis (ARN) syndrome but follows a chronic course similar to CMV retinitis, which may cause misdiagnosis.
Syphilitic hemorrhagic necrotizing retinitis can mimic CMV retinitis; all patients should undergo treponemal testing.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Ho M, Invernizzi A, Zagora S, et al. Presenting Features, Treatment and Clinical Outcomes of Cytomegalovirus Retinitis: Non-HIV Patients Vs HIV Patients. OcularImmunology and Inflammation. 2019;29:535-542.
- Schneider EW, Elner SG, van Kuijk FJ, et al. Chronic retinal necrosis: cytomegalovirus necrotizing retinitis associated with panretinal vasculopathy in non-HIV patients. Retina. 2013;33(9):1791–1799.
- Rissotto F, Scandale P, Miserocchi E. Ocular syphilis masquerading as CMV retinitis in a transplanted patient. Eur J Ophthalmol. 2023 Oct 10:11206721231206441.
- John, G.T., Manivannan, J., Chandy, S., Peter, S., and Jacob, C.K. Leflunomide therapy for cytomegalovirus disease in renal allograft recepients. Transplantation. 77:1460–1461, 2004.
- Levi, M.E., Mandava, N., Chan, L.K., Weinberg, A., and Olson, J.L. Treatment of multidrug-resistant cytomegalo- virus retinitis with systemically administered leflunomide. Transpl. Infect. Dis. 8:38–43, 2006.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE


