CASE REPORT
A 48-year-old female patient presented with a four-month history of painless loss of vision in her left eye.
There was no significant medical history. An ophthalmic examination revealed a best-corrected visual acuity of 20/20 in the right eye and a reduced visual acuity of 20/320 in the left one.
In both eyes, intraocular pressure was 14 mmHg, the anterior segment was unremarkable, and there was no relative afferent papillary defect.
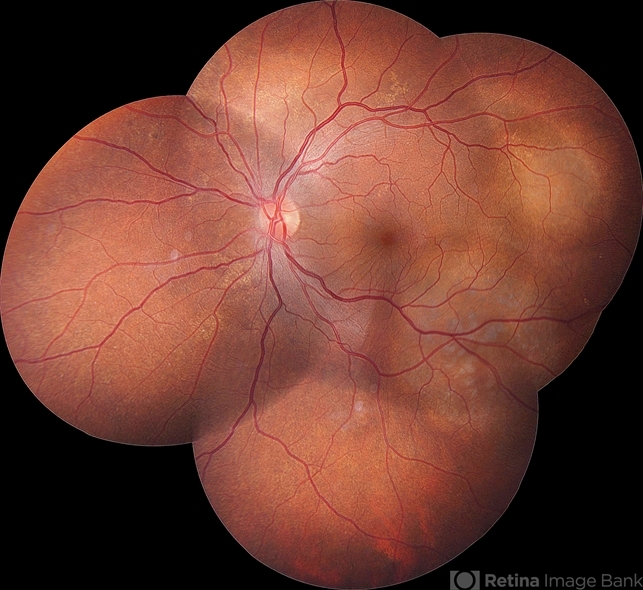
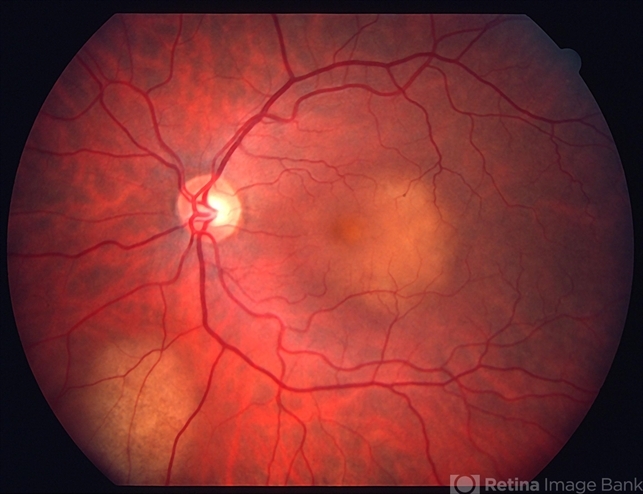
Fundus examination revealed a yellowish-white, elevated choroidal mass measuring around 6 disc diameters along the superior-temporal arcade associated with overlying retinal pigment epithelium (RPE) alterations in the right eye and a large subretinal mass involving the posterior pole with exudative retinal detachment in the left eye.
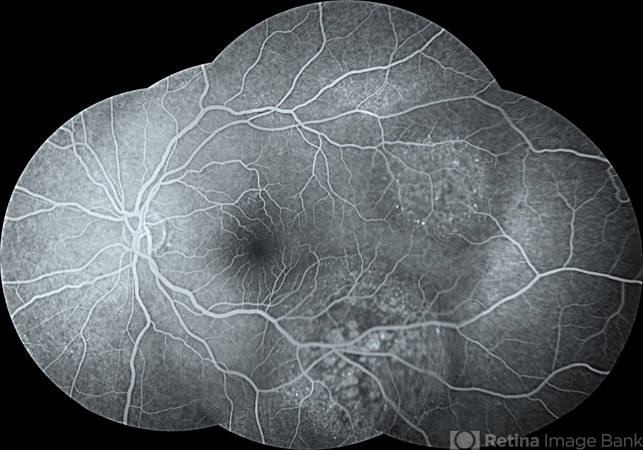
Fundus fluorescein angiography revealed initial hypofluorescence of lesions that changed over time to heterogeneous hyperfluorescence in both eyes.
The B scan ultrasonography results were unremarkable in the right eye and revealed a choroidal mass with high internal reflectivity, and associated exudative retinal detachment in the left eye.
A swept-source optical coherence tomography (SS-OCT) of the macula showed normal findings in the right eye and the presence of subretinal fluid involving the fovea in the left eye.
SS-OCT of choroidal lesions revealed a dome-shaped elevation of the neurosensory retina and RPE with adjacent subretinal fluid in the left eye.
Based on the clinical findings, it was hypothesized that the patient was presenting with choroidal metastasis.
Choroidal Metastases DISEASE entity
The uvea is the most common site for ocular metastasis. Within the uvea, 88% of metastases are to the choroid, followed by metastases to the iris (9%) and ciliary body (2%).
This large difference is thought due to the distribution of blood supply, which heavily favors the choroid as compared to the iris or ciliary body.
Shields and associates published a comprehensive survey of uveal metastases in 520 eyes of 420 patients with a total of 950 uveal metastases.
The most common primary cancer sites for uveal metastasis in males were lung (40%), gastrointestinal (9%), kidney (8%), and other. Rarely, serous retinal detachment is the first manifestation of aggressive malignancies, such as testicular cancer.
Choroidal Metastases Diagnosis
Physical examination:
Choroidal metastases are typically yellow in color, have a plateau configuration, and are associated with subretinal fluid. They can be solitary and unilateral or multiple and bilateral.
Ultrasound can play a key role in making the diagnosis of a large choroidal metastasis as the internal reflectivity is variable (high and intermediate) compared to melanoma in which the internal reflectivity is low.
Symptoms:
Patients with choroidal metastases present to ophthalmologists with visual symptoms almost in 90% of cases. Asymptomatic metastases are commonly detected in the fellow eye.

Patients most often present with blurred vision (70%), flashes and floaters (12%), and pain (7%). It is not uncommon for metastases to be found in asymptomatic patients.
Diagnostic procedures:
Indocyanine green angiography shows a blockage of the background staining and a patchy staining of the tumor surface. Intratumoral vessels could not be detected using ICG-A.
Optical coherence tomography may reveal a pattern of hyperintense irregular spots in the context of the photoreceptor layer and in the retinal pigment epithelium, subretinal fluid, and marked irregularity of the retinal pigment epithelium with thickening and gross undulation.
Ultrasound, fine needle aspiration biopsy (FNAB), and fundus autofluorescence are all used to aid in the diagnosis of choroidal metastases.
Ultrasound can be very useful in diagnosis. A-scan will typically show moderate to high internal reflectivity. B-scan will identify an echogenic choroidal mass and may show secondary retinal detachment.
Choroidal metastases are characterized by a significantly lower height-to-base ratio than melanomas, whereas reflectivity is significantly higher in metastases.
Color flow mapping shows that choroidal metastases tend to have hyper-vascularity, lack a ‘dominant vessel’, and typically have a ‘peripheral pattern’ blood flow.
Differential diagnosis
Choroidal Metastases MANAGEMENT
Regarding treatment of choroidal metastases, it is important to first assess the patient’s systemic status. This can be done with a thorough history, physical exam, laboratory evaluation, and imaging studies.
It is also important to assess the condition of the opposite eye and examine for multifocality of tumors.
General treatment
Treatment for choroidal metastases includes systemic chemotherapy and/or hormonal therapy as well as plaque radiotherapy, external beam radiation therapy (EBRT), and/or photodynamic therapy.
Treatment involves a collaborative effort between the ocular oncologist, radiation oncologist, and medical oncologist. Sometimes, it can be difficult to convince the medical oncologist that the patient has metastatic disease.
If the patient does not have known metastatic disease then a PET CT is often warranted to evaluate for metastasis elsewhere in the body.
If no other lesions are found then a biopsy may be requested from the oncologist. If other metastases are found then sometimes chemotherapy alone can treat the choroidal metastasis with complete resolution.
Plaque radiotherapy is usually reserved for solitary metastases. This modality offers precise, controlled radiation delivery to the eye.
Furthermore, it is a quick treatment modality, requiring only 3 to 4 days of treatment, as compared with EBRT, which may require 3 to 4 weeks of therapy.
Treatment duration is an important consideration in uveal metastases and must be weighed with life expectancy.
Several considerations should be taken into account when designing plaque radiotherapy and radiation exposure time.
These include the size and thickness of the metastasis, the distance of the lesion from the optic nerve, and the distance of the lesion from the foveola.
Complications from plaque radiotherapy are similar to those of external beam and other radiation therapies, including radiation retinopathy, papillopathy, and cataracts.
These side effects are uncommon, especially given the short life expectancy of many patients.
External beam radiation works well for bilateral and multifocal diseases and can diminish the exudative detachment often associated with these lesions thereby improving vision.
Photodynamic therapy (PDT) can also be used to treat small metastases in the posterior choroid. When associated with SRF and decreased vision, PDT often improves vision after treatment.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Phelps, P. O., et al. “Metastatic mixed germ-cell neoplasm presenting as retinal detachment.” Journal of clinical oncology: official journal of the American Society of Clinical Oncology 30.13 (2012): e133.
- Krause L, Bechrakis NE, Kreusel KM, Servetopoulou F, Heinrich S, Foerster MH. Indocyanine green angiography in choroid metastases. Ophthalmologe. 2002 Aug;99(8):617-9.
- Iuliano L, Scotti F, Gagliardi M, Bianchi I, Pierro L. SD-OCT Patterns of the Different Stages of Choroidal Metastases. Ophthalmic Surgery, Lasers and Imaging Retina.2012;43:E30-E34.
- Sobottka B, Schlote T, Krumpaszky HG, Kreissig I. Choroidal metastases and choroidal melanomas: comparison of ultrasonographic findings. British Journal of Ophthalmology.03/1998;82(2):159-61.
- Neudorfer M, Waisbourd M, Anteby I, Liran A, Goldenberg D, Barak A, Kessler A. Color flow mapping: a non-invasive tool for characterizing and differentiating between uveal melanomas and choroidal metastases. Oncology reports 2011;25;91-96.
- Shields CL, Shields JA, Gross N, Schwartz G, Lally S. Survey of 520 eyes with uveal metastases. Ophthalmology, 1997;104:1265-76.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

