CASE REPORT
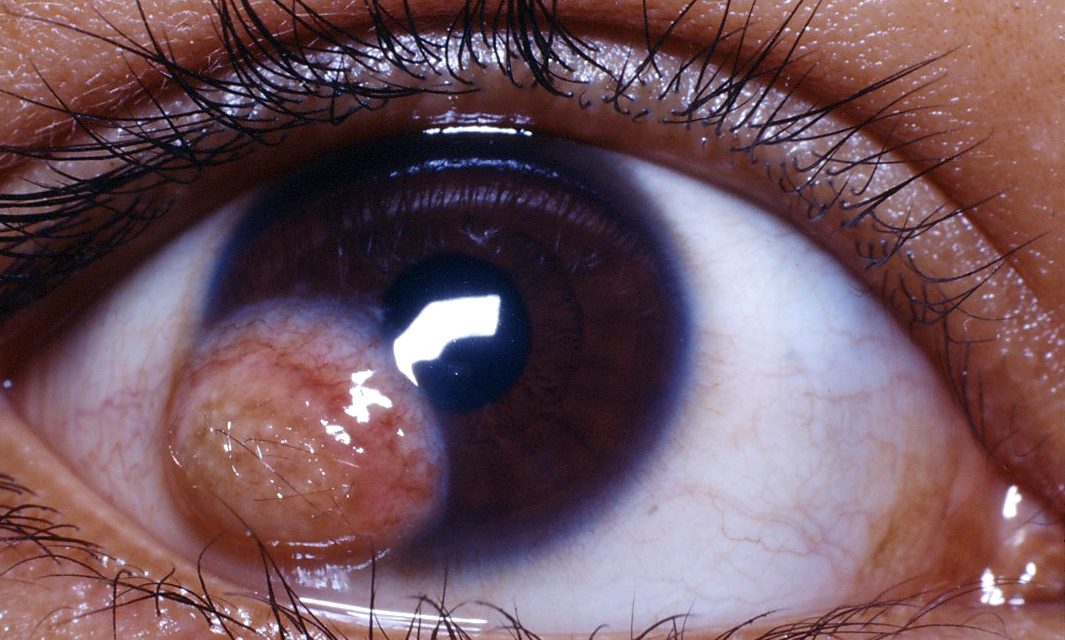
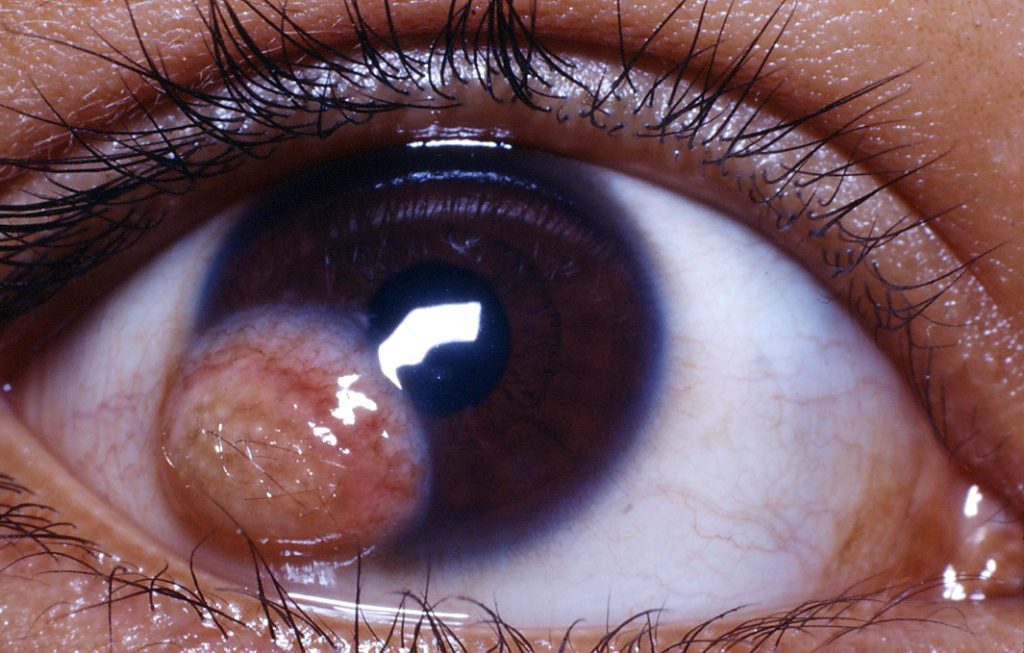
A 6-month-old infant was referred to an ophthalmology clinic due to a conspicuous white, raised lesion on the cornea of the right eye, with no reported family history of ocular abnormalities or complications during pregnancy.
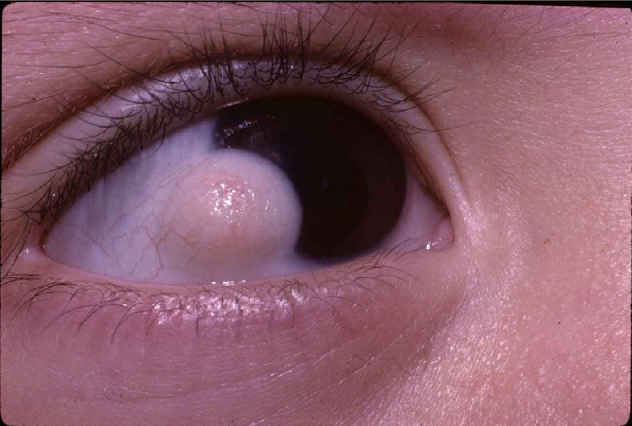
During the clinical examination, an ophthalmologist identified a well-defined, non-vascularized mass on the cornea measuring approximately 4 mm in diameter, showing characteristics such as hair follicles and sebaceous glands.
Assessing visual acuity in the affected eye proved challenging due to the patient’s age.
To further investigate, corneal imaging, including anterior segment optical coherence tomography (AS-OCT) and ultrasound biomicroscopy (UBM), was conducted to determine the depth and extent of the lesion, ultimately confirming the diagnosis of a corneal dermoid.
Corneal Dermoid DISEASE entity
A corneal dermoid is a benign congenital choristoma (growth of microscopically normal tissue in an abnormal location) on the anterior surface of the eye.
It is also called limbal dermoid and epibulbar demoid. It frequently presents as a whitish or yellowish lesion at the corneal limbus, though limbus-sparing dermoids and dermoids involving the entire cornea have been reported.
Importantly, corneal dermoids and orbital dermoid cysts are two separate disease entities. Several systemic conditions and other syndromes have been associated with corneal dermoids.
Goldenhar syndrome:
Also called oculo-auriculo-vertebral spectrum and facio-auriculo-vertebral dysplasia, Goldenhar syndrome is characterized by the classic triad of mandibular hypoplasia resulting in facial asymmetry, ocular and auricular malformations, and vertebral anomalies.
Ocular malformations may include corneal dermoids, microphthalmia, and coloboma. Most cases of Goldenhar syndrome are sporadic, but familial cases have been reported.
Ring dermoid syndrome:
Ring dermoid syndrome is a rare syndrome with autosomal dominant inheritance characterized by bilateral annular limbal dermoids.
Additional clinical findings include conjunctival keratinization, hairs, and corneal lipid deposition. No extraocular anomalies have been reported. Mutations in PITX2 have been associated with ring dermoid syndrome.
Epidermal nevus syndromes:
Epidermal nevus syndromes are a group of rare disorders characterized by the presence of skin lesions known as epidermal nevi and extra-cutaneous abnormalities, most often affecting the brain, eye, and skeletal systems.
Ocular abnormalities may include corneal dermoids, cataracts, and colobomas. Of note, sebaceous nevus syndrome, a type of epidermal nevus syndrome, is known to have malignant potential.
Other associations:
Corneal dermoids may present with a variety of ocular abnormalities and extraocular abnormalities. Examples include scleral/corneal staphyloma, aniridia, aphakia, cataract, microphthalmia, coloboma of the upper eyelid, lacrimal stenosis, nevus flammeus, neurofibromatosis, Treacher Collins syndrome, and Duane syndrome.
MANAGEMENT of Corneal Dermoid
Corneal dermoids have been traditionally classified into three grades to help guide clinical and surgical management. Grade I corneal dermoids are superficial lesions measuring less than 5mm and localized to the limbus.

Grade II corneal dermoids are larger lesions covering most of the cornea and extending deep into the stroma down to the Descemet membrane without involving it.
Grade III corneal dermoids are large lesions covering the whole cornea and extending through the structures between the anterior surface of the eye and the pigmented epithelium of the iris. In general, only small asymptomatic Grade I dermoids may be medically managed.
Medical management
Medical management is appropriate for Grade I dermoids that induce only mild astigmatism of < 1D with minimal surface irregularity and good patient adherence to spectacle correction.
In these cases, close clinical observation with serial examinations in a clinic is recommended. The serial examinations should be performed once every 6-12 months and should include visual acuity, measurement of the lesion, stereopsis, and cycloplegic refraction.
In the presence of suspected or proven amblyopia, vision should be monitored every 4 months, and treatment with spectacles and occlusion therapy should be attempted.
Surgery carries the risk of postoperative scarring and development of pseudopterygium.
Surgical management
Surgery is indicated in patients with grade I limbal dermoids if they have the following conditions.
- Chronic eye rubbing due to irritation and recurrent conjunctivitis
- Amblyopia unresponsive to medical management
- Progressive dellen with corneal surface decompensation
- Growth and encroachment into the pupillary area or optical zone
- Aesthetic considerations
- Inadequate lid closure
Surgery is universally indicated for grade II and III limbal dermoids.
A variety of surgical approaches to corneal dermoids have been described in the literature. A comprehensive review of the literature by Pirouzian generated the following recommendations:
- Grade I, <50 μm thickness and <1 mm diameter*: simple excision
- Grade I, <100 μm thickness and <1 mm diameter*: keratectomy + amniotic membrane transplantation + autologous limbal stem cell allograft
- Grade II and deeper Grade I: keratectomy + amniotic membrane transplantation + limbal stem cell allograft + pericardial patch graft versus anterior or deep anterior lamellar keratoplasty ± amniotic membrane transplantation
- Grade III: total anterior segment reconstruction
*Corneal dermoids of such small size were rarely observed in our clinical practice.
Additionally, optical iridectomy is frequently needed in staged surgical management to permit visual development in the absence of a clear cornea.
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Hameed S, Kaur I, Singh V, Mishra DC, Reddy JC. Congenital central corneal dermoid: A rare entity. European Journal of Ophthalmology. 2022;32(3):NP5-NP9. doi:10.1177/1120672120986365
- Liu J, Liang L. A giant corneal dermoid. BMJ. 2018;362:k3200. doi:10.1136/bmj.k3200
- Baum JL, Feingold M. Ocular Aspects of Goldenhar’s Syndrome. American Journal of Ophthalmology. 1973;75(2):250-257. doi:10.1016/0002-9394(73)91020-9
- Mattos J, Contreras F, O’Donnell FE. Ring dermoid syndrome. A new syndrome of autosomal dominantly inherited, bilateral, annular limbal dermoids with corneal and conjunctival extension. Arch Ophthalmol. 1980;98(6):1059-1061. doi:10.1001/archopht.1980.01020031049007
- Xia K, Wu L, Liu X, et al. Mutation in PITX2 is associated with ring dermoid of the cornea. Journal of Medical Genetics. 2004;41(12):e129-e129. doi:10.1136/jmg.2004.022434.
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE