CASE REPORT
A 35-year-old male presented to an ophthalmology clinic reporting persistent headaches, blurred vision, and occasional halos around lights in his left eye, following a significant head injury from a car accident two months prior.
Despite receiving medical attention for the head injury, ocular symptoms gradually emerged over the past few weeks.
Initial examination revealed visual acuity of 20/20 in the right eye and 20/40 in the left eye, with elevated intraocular pressure at 30 mmHg.
Slit-lamp examination and gonioscopy indicated an irregular and widened anterior chamber angle in the left eye, prompting suspicion of Angle Recession Glaucoma.
The diagnostic challenges stemmed from the subtle and progressive nature of the condition, with the delayed onset of symptoms and initially inconspicuous signs leading to an oversight.
Crucial diagnostic clues were later identified through additional tests, including optical coherence tomography revealed thinning of the neuroretinal rim, and visual field testing demonstrating a characteristic pattern of glaucomatous visual field loss.
The comprehensive approach involving clinical examination, gonioscopy, OCT, and visual field testing confirmed the diagnosis of Angle recession glaucoma (ARG).
DISEASE
Angle recession glaucoma (ARG) is a secondary open-angle glaucoma that is associated with ocular trauma.
Recession of the anterior chamber angle is a common slit lamp and gonioscopic finding following concussive ocular trauma.
A small percentage of these people go on to develop glaucomatous optic neuropathy and vision loss days, months, or even years later. There are reports of glaucoma developing up to 50 years after the injury.
Angle recession was first described by Collins in 1892. The association between trauma and unilateral glaucoma was made by D’Ombrain in 1949.
However, it was not until 1962 that Wolf and Zimmer correlated trauma with angle recession and subsequent glaucoma in a case series of six patients.
It has been reported that up to 60% of eyes with non-penetrating or concussive trauma will develop some degree of angle recession.
Angle recession is also strongly associated with traumatic hyphema with studies reporting a 60-100% incidence. The most commonly reported forms of trauma associated with Angle recession glaucoma (ARG) are recreational activities and assault.
However, a portion of patients never recall a specific event despite other clinical signs of trauma such as iris sphincter tears or traumatic cataracts.
Diagnosis
Physical examination
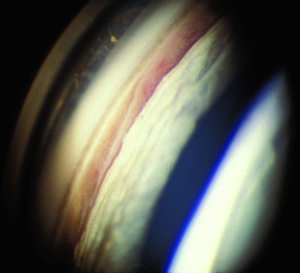
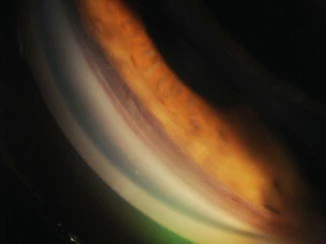
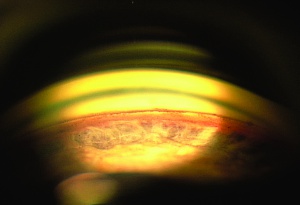
Gonioscopy:
The key exam finding in angle recession is the widening of the ciliary body band which is seen on gonioscopy. This exam finding, in the presence of elevated pressure and nerve damage, leads to the diagnosis of Angle recession glaucoma (ARG).
Some normal eyes have a broad ciliary body band thus it is important to compare suspected areas of recession to the opposite eye to see what the “normal” ciliary body band looks like to avoid mistaking physiologic or even 360-degree recession as normal.
Patients with significant contusion injuries such as hyphema should have a gonioscopy every year to assess for angle recession.
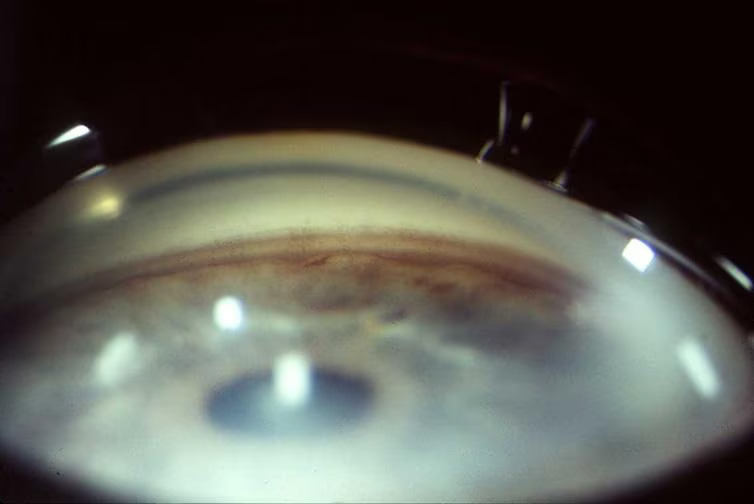
Slit Lamp Exam:
Other evidence of ocular trauma should clue the clinician to look for angle recession. Such findings might include iris sphincter tears, corneal scars, Vossius ring, iridodialysis, iridodenesis, phacodenesis, and hyphema.
MANAGEMENT
Treatment for ARG is generally the same as for primary open-angle glaucoma save for a few exceptions noted below.
Medical therapy
Topical aqueous suppressants are effective including beta-blockers, carbonic anhydrase inhibitors, and alpha agonists.
Prostaglandin analogs should be avoided in the acute phase of trauma because of their potential to be pro-inflammatory.
However, prostaglandin analogs have the theoretical benefit of bypassing the dysfunctional trabecular meshwork by increasing uveoscleral outflow and can be used after the acute phase is over.
Pilocarpine should be avoided as it has been reported to exacerbate angle recession. If pupillary block is present from lens dislocation, cycloplegics may be helpful until surgery is performed.
Surgical Therapy
Argon laser trabeculoplasty in small case series has yielded rather unsatisfactory results and fails to lower the IOP long-term in this group of patients.
An analysis of Selective Laser Trabeculoplasty among 560 patients in the IRIS registry found the failure rate was 48% at 18 months, whereas the failure rate overall (79,332 lasers) was 41%.
Trabeculectomy with MMC has shown to be successful in lowering IOP in ARG. However, patients with ARG have demonstrated an increased risk of failure after trabeculectomy.
Glaucoma drainage devices have demonstrated some benefit, though their success rates are lower than with other types of glaucomas. Cyclodestructive procedures may be an alternative option for eyes with limited visual potential.
Angle recession glaucoma (ARG) is generally more difficult to control medically and surgically than other types of glaucomas. Patients should be adequately counseled and follow-up examinations should be performed regularly.
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Kaufman J, Tolpin D. Glaucoma after traumatic angle recession. Am J Ophthalmol. 1974;78:648–654.
- Spaeth GL. Traumatic hyphema, angle recession, dexamethasone hypertension, and glaucoma. Arch Ophthalmol. 1967;78:714–721.
- Collins ET. On the pathological examination of three eyes lost from concussion. Trans Ophthalmol Soc UK. 1892;12:180–186.
- D’Ombrain. Traumatic or concussion chronic glaucoma. Br J Ophthalmol. 1949;33:395–400.
- Herschler J. Trabecular damage due to blunt anterior segment injury and its relationship to traumatic glaucoma. Trans Am Acad Ophthalmol Otolaryngol .1977;83:239.
- Blanton FM. Anterior chamber angle recession and secondary glaucoma: a study of the after-effects of traumatic hyphemas. Arch Ophthalmol. 1964;72:39–44.
- Filipe JA, Barros H, Castro-Correia J. Sports-related ocular injuries. A three-year follow-up study. Ophthalmology. 1997;104(2):313–318.
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE

