CASE REPORT
A 60-year-old female presented to an ophthalmology clinic complaining of sudden vision loss and distorted vision in the right eye, six months after undergoing uneventful cataract surgery.
She described a sudden onset of visual impairment accompanied by floaters and a sensation of movement in the affected eye, denying any recent trauma, ocular injury, or systemic illnesses.
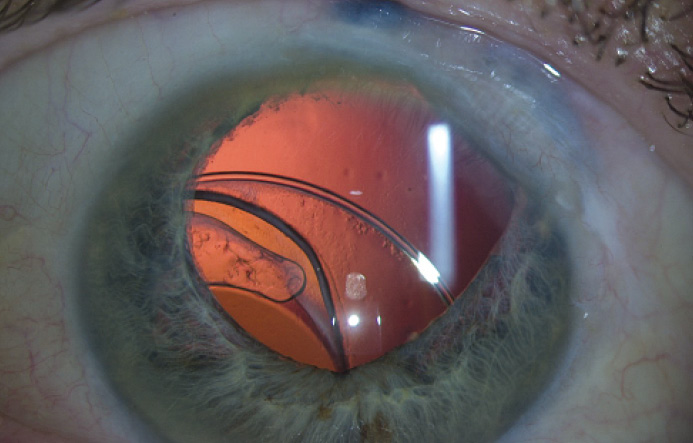
During ocular examination, her visual acuity in the right eye was reduced to counting fingers at one foot. Slit-lamp examination revealed a visibly displaced intraocular lens (IOL) into the vitreous cavity, with no signs of inflammation or increased intraocular pressure.
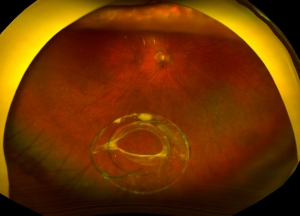
Additional diagnostic tests, including ultrasound biomicroscopy and optical coherence tomography (OCT), confirmed the dislocation of the intraocular lens and revealed vitreous prolapse.
Consequently, the patient was diagnosed with a dislocated intraocular lens in the right eye.
Dislocated intraocular lens (IOL) DISEASE entity
Dislocated intraocular lens (IOL) is a rare, yet serious complication whereby the intraocular lens moves out of its normal position in the eye.
IOL dislocation has been reported at a rate of 0.2% to 3%. It may occur as a result of an early or late complication of cataract surgery, prior vitreoretinal surgery, trauma, or an inherent pathological process or connective tissue disorder contributing to lens zonular weakness.
Dislocation may present as phacodonesis, simple decentration within the bag or in the sulcus, partial subluxation, or complete dislocation of the lens within and outside of the bag.
Decentration usually refers to loss of IOL centration without zonular or capsular instability. Subluxation refers to partial zonular or capsular instability.
Dislocation is due to total zonular or capsular instability. However, the terms are commonly interchanged. Once the dislocated IOL is identified, there are several possible management options.
IOL dislocation is typically related to the integrity of the capsular bag and its support system (zonules) and their ability to support an IOL.
There are many predisposing conditions that increase the risk of capsular bag instability and zonular weakness including cataract surgery, prior vitreoretinal surgery, aging, axial myopia, inflammation/uveitis, trauma, retinitis pigmentosa, diabetes mellitus, atopic dermatitis, mature cataract, previous episodes of acute angle-closure attack, connective tissue disorders e.g. pseudoexfoliation syndrome (being the most common risk factor with more than 50% of cases), Marfan syndrome, homocystinuria, hyperlysinemia, Ehlers-Danlos Syndrome, scleroderma, Weill-Marchesani syndrome, ectopia lentis.
Dislocated intraocular lens (IOL) Diagnosis
History, signs, and symptoms:
Given that many predisposing conditions increase the risk of IOL dislocation, a thorough history is necessary in patients.
Patients with a dislocated IOL may experience a decrease or change in vision, diplopia, and/or glare.
Additionally, they may report ocular pain or headaches from intermittent angle closure and/or inflammation. Some patients also report seeing the edge of the IOL.
Diagnostic procedures:
A complete ophthalmologic exam is necessary in the diagnosis of a dislocated IOL including an anterior and posterior segment exam.

A detailed dilated retinal exam with scleral depression is important. If a detailed exam is not feasible, Bscan echography and/or an anterior segment OCT/ultrasound biomicroscopy (UBM) may be helpful in evaluating a posteriorly dislocated lens behind the iris in the anterior aspect of the vitreous cavity.
Types of Dislocated intraocular lens (IOL)
IOL dislocation may present as phacodonesis, simple lens decentration within an intact capsular bag or in the sulcus, partial lens subluxation out of the capsular bag, or complete dislocation of the lens within or outside of the bag into the anterior or posterior chamber.
If there is a posterior capsule defect or tear, the IOL may slide out of the bag, hence out-of-the-bag dislocation.
If there is a defect in the stability of the capsular bag support system e.g. zonular weakness, the entire IOL with the capsular bag may dislocate, hence in-the-bag dislocation.
MANAGEMENT
Observation may be a possible management option in cases where IOL subluxation is minimal without a significant impact on vision and damage to surrounding ocular structures.
Those with pseudophacodonesis and without inferior dislocation are usually asymptomatic and tend to be such candidates.
In such cases, refraction may help sharpen the patient’s vision with close monitoring thereafter. Close follow-up is imperative to ensure patients do not develop potential IOL dislocation sequelae that may necessitate surgical intervention.
In cases where vision is affected and/or there is damage to surrounding ocular structures, surgery plays a large role in IOL dislocation management.
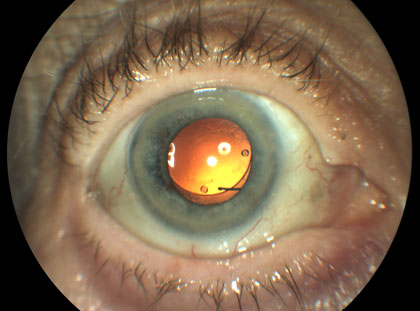
The most common indications for surgery are decreased visual acuity, monocular diplopia, and halos. Less commonly, retinal detachment, glaucoma, and/or uveitis-Glaucoma-Hyphema (UGH) syndrome portend surgical intervention.
Several surgical options exist in the management of dislocated IOL and should be tailored to each individual.
Surgery typically includes pars plana vitrectomy to remove the dislocated lens with either an IOL cutter or through a scleral tunnel or sclerocorneal incision. This is followed by secondary IOL implantation.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Stark, W.J., Jr., et al., Intraocular lenses: complications and visual results. Trans Am Ophthalmol Soc, 1983. 81: p. 280-309.
- Stark, W.J., et al., The FDA report on intraocular lenses. Ophthalmology, 1983. 90(4): p. 311-17.
- Kratz, R.P., et al., The Shearing intraocular lens: a report of 1,000 cases. J Am Intraocul Implant Soc, 1981. 7(1): p. 55-7.
- Gimbel, H.V., et al., Late in-the-bag intraocular lens dislocation: incidence, prevention, and management. J Cataract Refract Surg, 2005. 31(11): p. 2193-204.
- Ascaso, F.J., V. Huerva, and A. Grzybowski, Epidemiology, Etiology, and Prevention of Late IOL-Capsular Bag Complex Dislocation: Review of the Literature. J Ophthalmol, 2015. 2015: p. 805706.
- Davis, D., et al., Late in-the-bag spontaneous intraocular lens dislocation: evaluation of 86 consecutive cases. Ophthalmology, 2009. 116(4): p. 664-70.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

