Ruptured Globe Management
Initial Care
Once the diagnosis is made, the ophthalmologist must arrange for immediate surgery, the sooner the better. Delays in surgical care can increase the risk of choroidal hemorrhage and/or endophthalmitis.
Preoperative protection against external pressure, with a fox shield, to reduce the risk of herniation of ocular contents through the rupture must be addressed.

Additionally, antiemetics should be given to reduce the risk of increased ocular pressure. Patients should receive prophylactic antibiotic treatment with vancomycin and ceftazidime to cover organisms commonly associated with posttraumatic endophthalmitis.
Tetanus status should be addressed and prophylaxis given if appropriate. Topical antibiotic corticosteroids and cycloplegics are administered to treat traumatic uveitis associated with the injury.
Surgery
Anesthesia:
General anesthesia is indicated in most cases. Local anesthesia is avoided because the volume of fluid instilled around the eye from a block may cause further prolapse of intraocular content, however, if a local block is performed, a retrobulbar block is most likely to provide good anesthesia with akinesia with a prudently small injection volume.
Initial Approach:
In most cases, the wound edge must first be cleaned of all materials whether they are external (foreign bodies, debris) or internal (intraocular tissue).
Following proper cleaning, repositioning is the goal except for vitreous prolapse which is preferably cut with the vitrectomy probe and every attempt should be made to preserve the iris even if the injury is over 24 hours old.
The only time when it is permissible to incarcerate tissue in the wound is when an expulsive choroidal hemorrhage occurs.
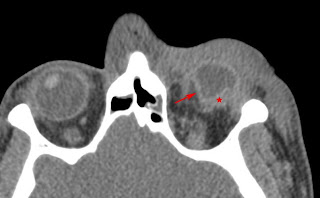
For occult globe rupture, during surgical exploration, a 360 peritomy is indicated to view all four quadrants of the posterior sclera bearing in mind that more than one rupture may be present.

Peritomy just anterior to the rectus muscle insertions provides a large circumferential conjunctival opening that facilitates exposure.
To allow control and gentle rotation of the eye for inspection, traction sutures are used first by buttonholing tenon fascia in each quadrant between rectus muscles and passing a 4-0 black silk or equivalent suture under and around the insertion of each rectus muscle without denuding the muscle sheaths to reduce scarring around the muscles.
Closure of the scleral wound:
If the scleral wound is anterior, it is best to carefully open the conjunctiva so that the entire length of the wound becomes visible.
Repairing the scleral defect is performed if possible using a 6-0 to 8-0 Vicryl or 8-0 to 9-0 nylon often using a spatula needle.
It is often desirable to place the first suture to close the middle of the rupture and subsequent sutures in the middle of the remaining defects or depending on the exposure of the operative site, defects can be closed by suturing progressively from one or both extremities of the rupture.
If the rupture is large, repair may be more detrimental where attempting such a posterior repair requires more force to rotate the globe which can increase extrusion of intraocular contents or risk an expulsive choroidal hemorrhage, the scleral wound is best left open.
These wounds may granulate spontaneously. After the conjunctiva is carefully closed, a shield is placed over the eye to prevent external pressure and the wound will close within days bearing in mind that the incarceration of tissues is the rule, not the exception, in these cases and must be addressed from the inside.
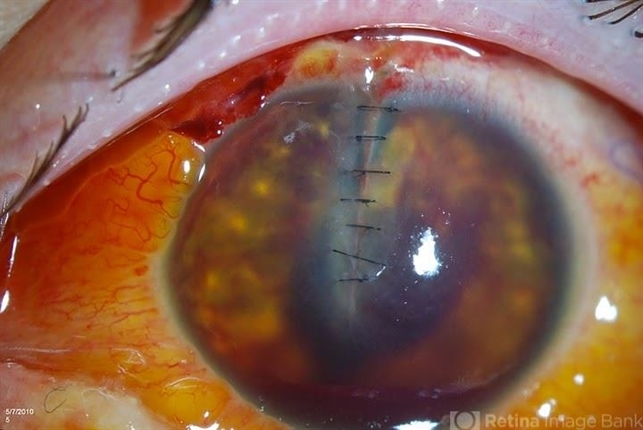
Closure of the corneal wound:
Suturing of this wound must be watertight and be as close to normal corneal anatomy as possible where scars will interfere with visual rehabilitation and edema interferes with vitreoretinal surgery.
Unless the wound is in the limbus, interrupted sutures should be used to avoid flattening the corneal dome shape with 10-0 nylon.
The suture should be 100% deep inside the anterior chamber to reduce corneal edema and minimize tissue shift or override. The surgeon should not grasp the cornea with forceps; the conjunctiva should be grasped if counterforce is needed. The 50% rule can be used primarily.
If the wound is angled, the first suture is placed at the angle and if the wound crosses the entire cornea, the Rowsey-Hays technique is recommended where sutures with large bites are first placed at the two ends followed by gradually smaller bites as the sutures approach the center in a centripetal fashion.
Eisner principle- Another variation of the suturing technique was suggested by Eisner to close a stellate laceration. In this, a purse-string suture is used to prevent trauma to spices of laceration, and a diamond knife is used for incising the corneal stroma to half the thickness at all the edges.
Further, 10-0 nylon sutures are passed through the adjacent stromal incision and the wound is closed with watertight opposition. The tightening opposes the central stroma and the apices of the laceration.
Closure of a Corneoscleral wound:
The initial suture is made at the limbus and should not be full thickness, followed by the closure of the corneal wound, followed by the closure of the scleral wound.
Vitreoretinal Surgery
Pars plana vitrectomy may be performed if indicated immediately after repair of the scleral rupture or often about 7-14 days depending on whether the closure of the scleral defect is watertight and on accompanying pathology.
Indications include dense vitreous hemorrhage, vitreous or retina incarcerated in the scleral rupture, retinal tears, and retinal detachment.
In cases where the rupture cannot be made watertight, up to about 2 weeks may be allowed for unrepaired posterior rupture to seal with early cicatrization and for choroidal detachments to recede while treating the eye with strong corticosteroid therapy and cycloplegia before attempting pars plana vitrectomy, however, there is also increasing evidence that an early pars plana vitrectomy may reduce risks of retinal detachment, scarring, and proliferative vitreous hemorrhage.
When performing the pars plana vitrectomy, great care must be taken to insert the infusion cannula into the vitreous and not into the supraciliary space underneath a ciliochoroidal detachment caused by preoperative hypotony with a longer than usual 6-mm cannula preferably or an AC maintainer can be used in these cases until the posterior view is clear enough to confirm placement of the pars plana infusion cannula.
If there is a metal intraocular foreign body and infection is suspected, surgery is performed as soon as possible with the determination of the incision site and pathway such as a previous wound, corneal scleral incision, and pars plana incision are made according to the foreign body feature, location, and disease characteristics.
A complete vitrectomy is performed via a pars plana incision avoiding the injury site. Retinotomy or retinectomy may be preferred according to trauma status and if the lens is not transparent enough, a lensectomy or phacoemulsification is performed first.
This study suggested the following for primary surgery;
(1) The prolapsed iris, choroid, and retina should be repositioned after complete irrigation and the prolapsed vitreous body can be removed otherwise retinal incarceration and closed tunnel detachment will result in poor visual acuity and severe proliferative response.
(2) The ends of the ocular rupture wound must be determined carefully and sutured completely to keep IOP normal.
(3) For patients with anterior chamber hyphema, anterior chamber irrigation after tamponade of viscoelastic could prevent blood staining of the cornea.
Postoperative and Follow-up
Eyes without watertight closure should be protected from external pressure for several weeks by a shield when glasses are not being worn.
Topical antibiotic is often administered in conjunction with topical corticosteroid and strong cycloplegia. A systemic antibiotic is not normally indicated with occult ruptures but is used if there is a laceration or perforation of the sclera or a more superficial defect that appears to be contaminated.
Theoretically, sympathetic ophthalmia can be reduced with several days of systemic corticosteroids, but this is a rare condition.
Silicone oil is removed 3 to 6 months postoperatively and artificial lens implantation is performed in patients with good corrected visual acuity.
Follow-up is often arranged for postoperative day 1, week 1, month 1, and month 3 depending on the course with more frequent follow-up for complications.
Every follow-up examination requires visual acuity, anterior segment, and posterior examination. Postoperative complications include secondary cataracts, belted corneal degeneration, iris atrophy, or irregular pupils.
Complications will vary depending on the extent of injury and mechanism. In addition to globe rupture, an orbital fracture, orbital hemorrhage, or orbital compartment syndrome can occur. Posttraumatic endophthalmitis occurs after penetrating trauma to the globe in 3 to 10 percent of cases.
For prevention in cases after open globe penetrating eye trauma, two days of systemic prophylactic antibiotics with intravenous vancomycin with either ceftazidime or ciprofloxacin after the penetrating eye injury if one is present.
In a review, a rate of 0.9% of endophthalmitis occurred following two days of prophylactic systemic antibiotics.
Prognosis
The Ocular Trauma Score is often used to predict the visual outcome of patients after open-globe ocular trauma ranging from 1 (most severe injury and worst prognosis at 6 months follow up) to 5 (least severe injury and least poor prognosis at 6 months) with globe rupture holding the worst prognosis followed by endophthalmitis, perforating injury, retinal detachment, and relative afferent pupillary defect in that order.
The Ocular Trauma Score is used by first determining the patient’s initial visual acuity after injury and their tissue diagnoses then subtracting raw points from each associated diagnosis/complication.
Then the raw score with the Ocular Trauma Score to estimate the patient’s probability of attaining a specific visual acuity range at a 6-month follow-up.
Posttraumatic endophthalmitis is associated with poor visual prognosis with visual acuities of 20/400 or better preserved only in 37% (75/210) of patients.
References
- Chronopoulos, A., Ong, J. M., Thumann, G. & Schutz, J. S. Occult globe rupture: diagnostic and treatment challenge. Surv Ophthalmol 63, 694–699 (2018).
- Kuhn F, Pelayes D. Management of the Ruptured Eye. European Ophthalmic Review 2009. 3(1):48-50.
- Weichel ED, Bower KS, Colyer MH. Chorioretinectomy for perforating or severe intraocular foreign body injuries. Graefes Arch Clin Exp Ophthalmol. 2010;248:319–330.
- McLean J. Steroid prophylaxis in sympathetic ophthalmia. Am J Ophthalmol. 1958;45:162e4.
- Andreoli CM, Andreoli MT, Kloek CE, et al. Low rate of endophthalmitis in a large series of open globe injuries. Am J Ophthalmol 2009; 147:601.
- Scott R. The Ocular Trauma Score. Community Eye Health. 2015;28(91):44–45.

RETINAL IMAGING BY YOUR SMARTPHONE

