Ruptured Globe entity
In ocular trauma, injuries can be initially classified as either closed globe or open globe where an open globe injury is defined as a full-thickness wound.
From there, an open globe injury can be described as secondary to blunt trauma or due to a laceration. A ruptured globe is classified as secondary to blunt trauma when an impact from a blunt object results in a momentary increase of the intraocular pressure resulting in an inside-out injury mechanism.

A laceration is classified as an open-globe injury that is full-thickness usually caused by a sharp object with the wound occurring at the impact site by an outside-in mechanism.
Furthermore, lacerations are defined as either a penetrating injury, intraocular foreign body, or a perforating injury. A penetrating injury is defined as a single laceration with no exit wound and if there is more than one entrance wound, each must be caused by a different agent.
An intraocular foreign body is defined as a retained foreign object causing an entrance laceration; of note, an intraocular foreign body is technically a penetrating injury but is grouped separately since there are different clinical implications due to the object.
A perforating injury is defined as two full-thickness lacerations both entrance and exit usually caused by a sharp object or projectile where both wounds are caused by the same agent.
The eye is filled with incompressible liquid and when a blunt object with sufficient momentum creates energy transfer over a large surface area, this greatly increases the intraocular pressure causing the eyewall to give way at its weakest point, which may or may not be at the impact site.
The actual wound is thus produced by an inside-out force and tissue herniation is very frequent and can be substantial. The site of rupture commonly occurs where the sclera is thinnest and weakest near the equator directly behind the insertion of the rectus muscles.
Other regions prone to rupture include the limbus, insertion of the optic nerve, and sites of prior eye surgery. Once a ruptured globe occurs, it may result in diffuse injury, hemorrhagic choroidal, and retinal detachment leading to a vigorous healing response that can lead to additional injury.
Rupture of the globe posterior to the spiral of Tillaux (surgical landmark delineated by connecting the rectus muscle insertions which approximate the underlying ora serrata) is normally accompanied by choroidal rupture and hemorrhage which may percolate through the retina to present as a vitreous hemorrhage.
Ruptured Globe Diagnosis
History:
Patients with a history of significant ocular and periocular blunt trauma should be considered ruptured until proven otherwise since the diagnosis can be difficult due to swelling and wounds may be occult. The mechanism of an injury must always be investigated.
A thorough review of medical/surgical history with a focus on prior surgery, trauma, and any previous or existing eye disease.
Physical Exam:
A complete ocular exam must be performed when possible starting with measurement of the visual acuity and testing for the presence of a relative afferent pupillary defect.

Next, gross confrontational visual field testing, identifying any relative difference in subjective brightness perception, and checking color vision should be performed.
If eye drops are necessary, prefer the use of new medication bottles and preservative-free variants. If clinical suspicion of a ruptured globe is high, any medication such as tetracaine or diagnostic eye drops such as fluorescein should be avoided.
Most open globe injuries can be diagnosed with a simple penlight examination; however, smaller wounds may require a slit-lamp examination for confirmation and to rule out associated injury, intraocular foreign body, and endophthalmitis.
In 74% of eyes, the wound is scleral or corneoscleral with typically a conjunctival wound. The following signs may help to establish the diagnosis: the presence of thick subconjunctival hemorrhage, scleral step sign, presence of a circumscribed mass under the conjunctiva from the expulsed lens, peaked pupil with the angle pointing toward the site of the scleral wound, loss of the iris, lens, or red reflex.
Of note, an occult globe rupture may be present without a visible scleral defect on the slit lamp. A deeper-than-normal anterior chamber with a posteriorly retracted plateau iris seen immediately after acute ocular trauma is pathognomonic of posterior globe dehiscence.
Additionally, extensive chemosis often hemorrhagic, relative hypotony, and vitreous hemorrhage may also be present in occult globe rupture.
If the presence of a wound is confirmed, evaluation should be stopped so that fine details of the injury are best determined during surgery to avoid causing additional tissue extrusion or bleeding.
Differential Diagnosis
- Traumatic hyphema
- Orbital fracture
- Closed-globe injury
- Laceration
- Penetrating injury
- Perforating injury
- Orbital compartment syndrome
Role of Imaging
In one study, CT evaluation was found to have accuracy, sensitivity, and specificity of 81%, 76%, and 85% respectively, so while CT is useful in cases of ocular trauma, particularly in cases of eyelid hematoma, swelling, intraocular hemorrhage, it can still not be solely relied on due to the potentially catastrophic consequences of an undiagnosed globe rupture.
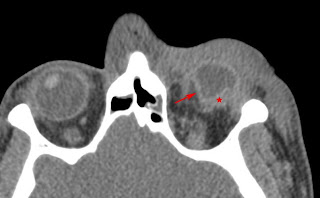
In a study evaluating the use of CT diagnosis of uncertain penetrating globe injuries, CT was found to not be a suitable alternative to surgical exploration which is still mandatory in unclear cases with findings of about one-third of unclear cases with rupture of the globe that were not diagnosed with CT evaluation.
For an initial assessment of orbital trauma, MRI is not recommended due to the potential of intraocular ferromagnetic objects and that MRI is insensitive regarding the visualization of foreign objects.
If globe rupture is suspected, many recommend proceeding directly to the operating room for exploration and skipping contact B-scan ultrasonography for concern for iatrogenic expulsion of globe contents.
In light of these studies on additional imaging modalities, a ruptured globe remains a clinical diagnosis based on history and physical examination.
MANAGEMENT of Ruptured Globe
Once the diagnosis is made, the ophthalmologist must arrange for immediate surgery, the sooner the better. Delays in surgical care can increase the risk of choroidal hemorrhage and/or endophthalmitis.
Preoperative protection against external pressure, with a fox shield, to reduce the risk of herniation of ocular contents through the rupture must be addressed. Additionally, antiemetics should be given to reduce the risk of increased ocular pressure.
Patients should receive prophylactic antibiotic treatment with vancomycin and ceftazidime to cover organisms commonly associated with posttraumatic endophthalmitis.
Tetanus status should be addressed and prophylaxis given if appropriate. Topical antibiotic corticosteroids and cycloplegics are administered to treat traumatic uveitis associated with the injury.
Read more about Ruptured Globe management strategies
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Kuhn F, Morris R, Witherspoon CD, et al. A standardized classification of ocular trauma. Ophthalmology 1996; 103:240.
- Duke-Elder S, MacFaul PA. Injuries: Part 1 Mechanical Injuries. In: System of Ophthalmology, CV Mosby, St. Louis 1972. Vol 14.
- Zeiter JH, Shin DH. Traumatic rupture of the globe after glaucoma surgery. Am J Ophthalmol 1990; 109:732.
- Lambrou FH, Kozarsky A. Wound dehiscence following cataract surgery. Ophthalmic Surg 1987; 18:738.
- Pieramici DJ. Open-globe injuries are rarely hopeless. Review of ophthalmology. 2005.
- Chronopoulos, A., Ong, J. M., Thumann, G. & Schutz, J. S. Occult globe rupture: diagnostic and treatment challenge. Surv Ophthalmol 63, 694–699 (2018).
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE

