CASE REPORT
A 34-year-old female presented with complaints of visual disturbances in her right eye, reporting intermittent blurry vision and a central scotoma for the past few weeks.
There was no significant family history of ocular diseases or known systemic health issues. Visual acuity in her right eye was 20/60, while her left eye was 20/20.
Clinical examinations, including slit-lamp evaluation, found clear corneas, unremarkable anterior chambers, and normal lens status in both eyes.
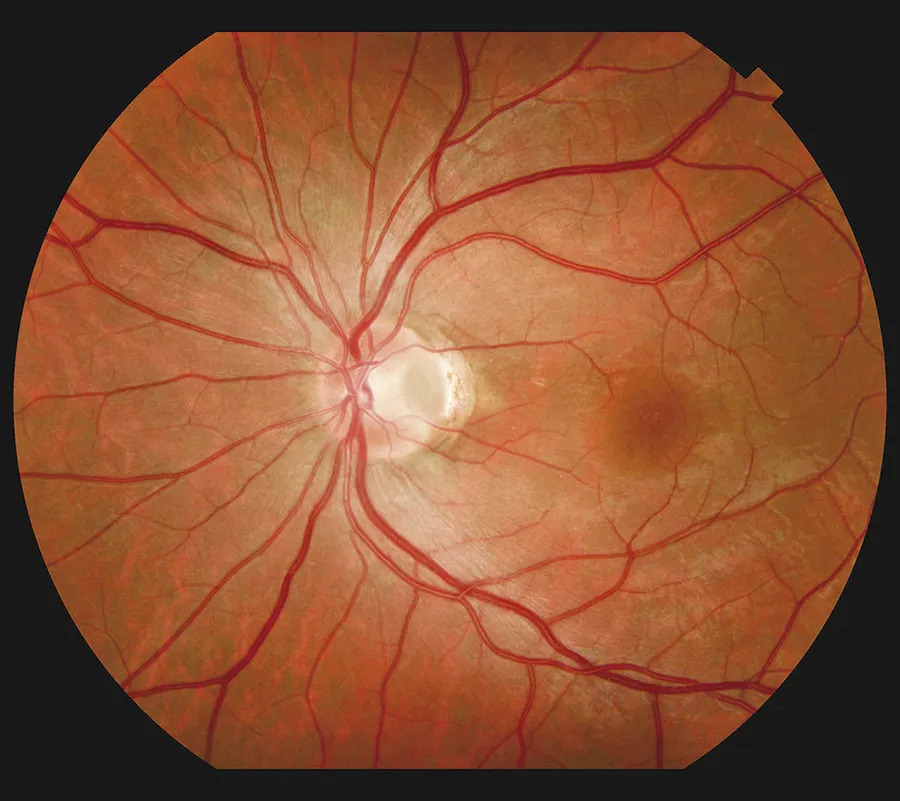
Fundus examination revealed a grayish-white, oval-shaped depression at the optic nerve head, consistent with an optic disc pit in her right eye.
Diagnostic tests, including Optical Coherence Tomography, Fundus Fluorescein Angiography, visual field testing, and B-scan ultrasonography, confirmed the diagnosis of Optic Pits.
Optic Pits DISEASE entity
Optic Pits (also known as optic nerve pits, optic disc pits, or less commonly optic holes) are congenital defects presumably arising from the failure of fetal fissure closure in embryogenesis.
Optic Disc Pits (ODP) were first described in 1882 by Wiethe in a 62-year-old female. Since that time, they have typically been an incidental finding on routine dilated fundus exams. Rarely, they may cause visual field defects or macular changes.
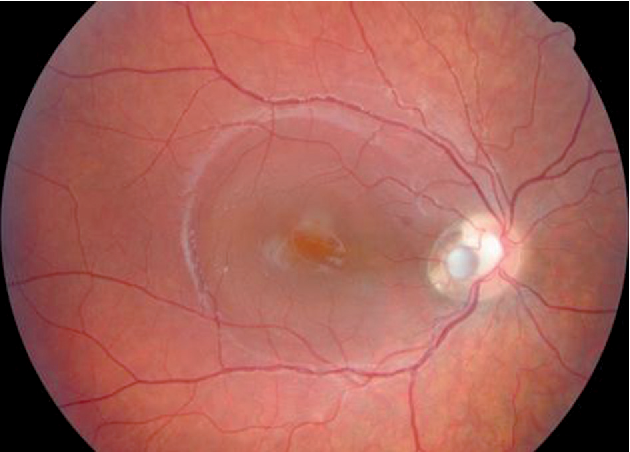
An ODP usually presents itself as a unilateral, solitary, ovoid, grey-white excavation of the optic disc most commonly in the inferotemporal quadrant of the nerve head.
15% of ODPs are thought to occur bilaterally. The size of the pit can occupy 1/8 -1/4 of the size of the disc. Depending on the optic disc size and location, they may cause arcuate field defects or enlarged blind spots.
Visual acuity is typically not affected unless macular involvement is present, either by a serous retinal detachment, retinal schisis, or cystoid macular edema. Patients with optic disc pit maculopathy initially notice a drop in visual acuity to around 20/70 in the affected eye.
Optic pits are thought to be a result of incomplete closure of the superior edge of the embryonic fissure. This has been the subject of some debate in the literature.
The mechanisms of subretinal fluid accumulation in optic disc pit maculopathy are not well understood. It has been postulated that the fluid may arise from one of several sources; the vitreous cavity, cerebrospinal fluid (CSF), the surrounding orbital space, or dural leaking vessels at the base of the pit.
As for the theory suggesting the fluid arising from the vitreous cavity, pre-existing vitreous traction on the macula and the optic disc is thought to play a role in the development of negative pressure with subsequent entrance of fluid through the ODP into the submacular space.

Whereas, the theory of CSF leaking into the macular schisis or subretinal space is thought to be from a direct communication of the subarachnoid space through the ODP that transmits fluid into the intra- and subretinal space.
MANAGEMENT of Optic Pits
The first treatment modality is observation especially if there is no macular involvement. The patient is made aware of his condition and counseled with regard to the possibility of vision loss.
Should the macula be affected, the treatment options include the following:
- laser photocoagulation: the objective of treatment includes repair of a serous detachment if it occurs as a complication of an optic nerve pit. The technique includes laser application temporal to the disc area to create a barrier for fluid not to enter the macula. Laser photocoagulation therapy has not had much success in most studies, patients treated did not notice improvement, and in fact, some reported more visual disturbance after the treatment.
- Surgical options: most commonly, a pars plana vitrectomy (PPV) is performed, with or without internal limiting membrane peel, with or without endo laser, and gas tamponade. The success of this method is based on the theory of vitreous traction leading to the formation of fluid (discussed earlier). Studies have shown promising long-term results in both retinal re-attachments (50-95% of patients) and visual improvement(>50% of patients).
An emerging surgical technique for managing ODPs is PPV combined with an inverted ILM flap to cover the optic disc and the ODP. This technique has shown promising results however evidence remains low due to the limited studies.
There are studies that reported high success rates with injecting gas tamponade with or without a barrier laser at the temporal disc edge. There was 50-75% fluid resolution and significant vision improvement, however, there was a need for re-injection of gas frequently due to recurrence.

A macular buckle is an option of treatment to promote reattachment of the macula via ab externo compression when detachment involves the macula.
This procedure is considered technically challenging despite the good anatomical and visual outcomes hence it is not widely applied.
Performing inner retinal fenestrations to create a passage for the fluid to travel to the vitreous has been reported, showing fluid resolution in 95%, and vision improvement in 56%.
Controlled active aspiration of the intraretinal fluid using a 38 gauge cannula for treatment of foveoschisis has been recently described.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Gordon R, Chatfield RK. Pits in the optic disc associated with macular degeneration. The British journal of ophthalmology. 1969;53(7):481–9.
- Optic disc pit: a review. Source: Graefe’s archive for clinical and experimental ophthalmology [0721-832X] Georgalas, Ilias yr:2011 vol:249 iss:8 pg:1113 -1122.
- Wang Y, Xu L, Jonas JB. Prevalence of congenital optic disc pits in adult Chinese: The Beijing Eye Study.
- Chatziralli I, Theodossiadis P, Theodossiadis GP. Optic disk pit maculopathy: Current management strategies. Vol. 12, Clinical Ophthalmology. Dove Medical Press Ltd; 2018. p. 1417–22.
- El Rayes EN, Habib AM, Soliman AH, Ibrahim OM, El Sawwah KMH. Novel Technique for Treatment of Foveoschisis Associated With Optic Disk Pits: Active Aspiration of Intraretinal Fluid. Retina. 2022 Jul 1;42(7):1406-1410.
- Annesley, W, Brown, G, Bolling, J, Goldberg, R, Fischer, D. “Treatment of retinal detachment with congenital optic pit by krypton laser photocoagulation.” Graefe’s Archive for Clinical and Experimental Ophthalmology 1987; 225:5.
- Brown, G, Tasman, W. Congenital anomalies of the optic disc. Grune & Stratton, New York 1983, p. 31.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE


