CASE REPORT
A 14-month-old male was referred to a pediatric ophthalmology clinic due to parental concerns regarding an ocular mass in the right eye, which had gradually increased in size over the past month, with no prior history of ocular or systemic illnesses and overall excellent health.
During the ophthalmic examination, the child exhibited normal visual behavior, though assessing detailed visual acuity was challenging due to his age.
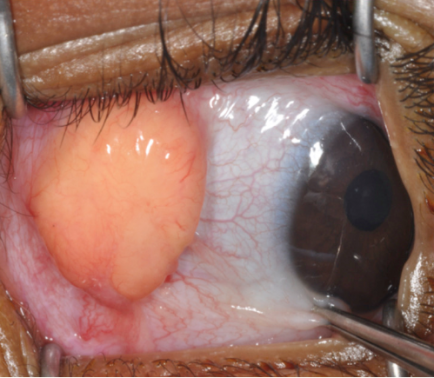
A firm, well-defined, yellowish-orange, subconjunctival mass, approximately 6 mm in diameter, was noted in the superior-temporal aspect of the right eye, with no apparent pain or discomfort.
The anterior segment examination of both eyes, including the cornea, anterior chamber, iris, and lens, was within normal limits. Fundus examination of the right eye revealed macular displacement due to the subconjunctival mass, while the left eye appeared normal.
Diagnostic procedures included B-scan ultrasound imaging of the right eye, revealing a well-defined, solid, subconjunctival mass with high internal reflectivity indicative of a solid tumor.
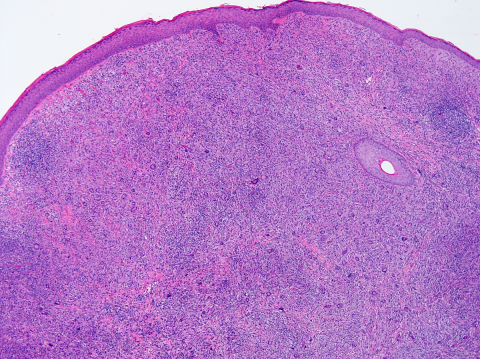
An incisional biopsy of the subconjunctival mass was performed under general anesthesia through histopathological examination, which showed a dense infiltrate of histiocytes and Touton giant cells within the lesion.
Additional imaging studies of other organs, including liver and spleen ultrasounds, were conducted to rule out systemic involvement, and these results returned normal.
Based on the clinical presentation, ophthalmic findings, and histopathological examination, the diagnosis of Juvenile Xanthogranuloma (JXG) was established.
Juvenile Xanthogranuloma (JXG) DISEASE entity
Juvenile xanthogranuloma (JXG) is a rare benign histiocytic proliferation that develops in infants and young children. JXG is the most common form of non-Langerhans cell histiocytoses. It is characterized by the presence of Touton giant cells.
JXG most commonly develops in infants younger than 2 years of age but has been found in older children. In a cohort of 174 JXG patients with cutaneous lesions, the mean age was 3.3 years (median 1 year).
In a cohort of 30 patients with ocular JXG, the mean age at diagnosis was 4.3 years (median 1.3 years)2. 0.3%-10% of patients with cutaneous JXG were reported to have ocular involvement with children under 2 years being at increased risk.
JXG has been reported to be more common in boys than in girls, with a male/female ratio ranging from 1.1:1 to 1.4:1.
However, in a cohort of 30 patients with ocular JXG, no gender predilection was shown. A large literature review found a 0.75% rate of systemic manifestations in patients with cutaneous JXG.
Juvenile Xanthogranuloma (JXG) Diagnosis
A diagnosis of Juvenile xanthogranuloma (JXG) is suspected in patients with characteristic yellowish cutaneous lesions. An excisional biopsy can be performed to confirm the diagnosis of the cutaneous eyelid or conjunctival lesions.
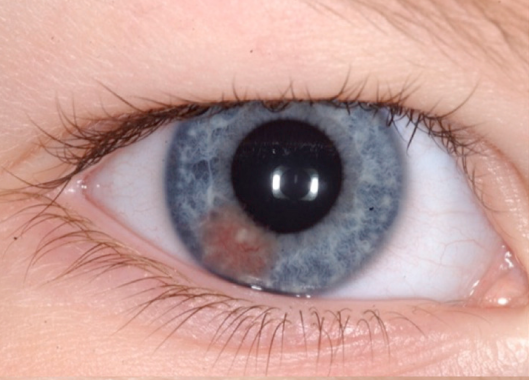
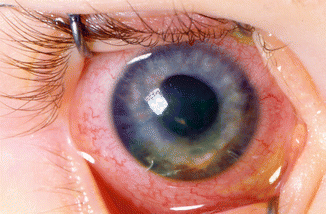
All patients with cutaneous Juvenile xanthogranuloma (JXG) are advised to have a complete ophthalmic examination. In cases of iris JXG, anterior segment optical coherence tomography can help confirm the diagnosis by demonstrating a thin, epi-iridic, flat mass.
Fine needle aspiration biopsy may be considered in cases that do not respond to corticosteroids or show atypical presentations concerning malignancy.
The classic histopathologic findings include multinucleated Touton giant cells in addition to epitheloid histiocytes, lymphocytes, and eosinophils (Figures 4-5). However, Touton giant cells are not mandatory for the diagnosis of JXG.
In early JXG, small- to intermediate-sized mononuclear histiocytes display a compact sheet-like infiltrate; the lipidization of histiocytes is not detectable and Touton giant cells are rarely found.
The pale eosinophilic cytoplasm is sparse to moderate and does often not contain any lipid vacuoles or only fine vacuoles.
Juvenile Xanthogranuloma (JXG) MANAGEMENT
For eyelid Juvenile xanthogranuloma (JXG), excisional biopsy is commonly performed and is both diagnostic and therapeutic. Alternatively, topical and intralesional corticosteroids have been used to treat eyelid lesions.
Topical corticosteroids have also shown success in the treatment of limbal JXG. Observation alone is a reasonable option for characteristic lesions, as most cutaneous lesions stabilize or regress in one to five years.
In a case report of a newborn with extensive JXG involving the orbit, sinuses, brain, and subtemporal fossa, management was limited to conservative observation. For iris JXG, prompt treatment is recommended to prevent vision loss from recurrent hyphema, secondary glaucoma, and complications related to neovascularization.
Corticosteroids are the mainstay for the treatment of iris JXG. Samara et al. reported the use of topical high-dose corticosteroids with a slow taper lasting 3 to 4 months.
Periocular corticosteroid injection was considered when the response to topical administration was poor or in case of concerns with compliance.
Systemic corticosteroid or low-dose ocular radiotherapy can be considered in recalcitrant cases. Multimodal chemotherapy has been used in rare cases of extensive, systemic JXG.
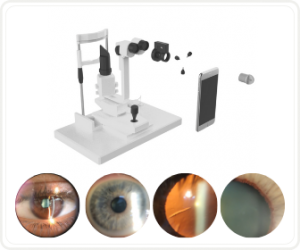
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Juvenile Xanthogranuloma. In: Basic and Clinical Science course (BCSC) Section 6: Pediatric Ophthalmology and Strabismus. San Francisco, CA: American Academy of Ophthalmology; 2017
- Samara WA, Khoo CT, Say EA, et al. Juvenile Xanthogranuloma Involving the Eye and Ocular Adnexa: Tumor Control, Visual Outcomes, and Globe Salvage in 30 Patients. Ophthalmology 2015;122(10):2130-8.
- DeBarge LR, Chan CC, Greenberg SC, et al. Chorioretinal, iris, and ciliary body infiltration by juvenile xanthogranuloma masquerading as uveitis. Surv Ophthalmol 1994;39(1):65-71.
- Wertz FD, Zimmerman LE, McKeown CA, et al. Juvenile xanthogranuloma of the optic nerve, disc, retina, and choroid. Ophthalmology 1982;89(12):1331-5.
- Hildebrand GD, Timms C, Thompson DA, et al. Juvenile xanthogranuloma with presumed involvement of the optic disc and retina. Arch Ophthalmol 2004;122(10):1551-5.
Slit-lamp Smartphone photography
RETINAL IMAGING BY YOUR SMARTPHONE