CASE REPORT
A 68-year-old male patient presented with a chief complaint of progressive vision loss in the left eye over six months. He had no history of ocular trauma, systemic diseases, smoking, or alcohol consumption.
His medical history included controlled hypertension. Initial examination indicated visual acuities of 20/20 in the right eye and 20/80 in the left eye, with normal intraocular pressure and unremarkable anterior segments in both eyes.
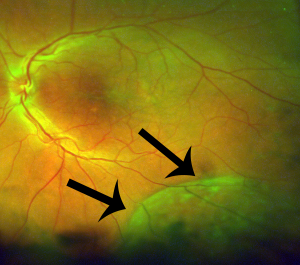
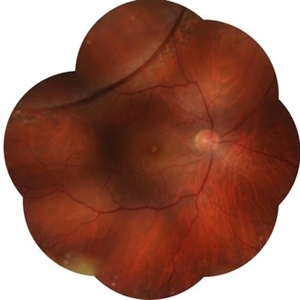
Smartphone fundoscopy of the left eye revealed characteristic retinal layer separation with a spoke-wheel pattern from the fovea.
Diagnostic assessments included Optical Coherence Tomography (OCT) confirming retinoschisis in the left eye, primarily affecting the outer plexiform and inner nuclear layers, Fundus Fluorescein Angiography (FFA) ruling out vascular abnormalities, and Electroretinography (ERG) indicating normal retinal function.
Consequently, the patient was diagnosed with senile retinoschisis in the left eye.
DISEASE
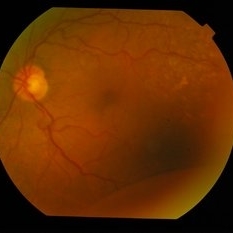
Senile retinoschisis, either acquired or degenerative, is a rare and hard-to-diagnose eye disease characterized by the abnormal separation of the neurosensory retina layers due to microcystic degeneration, typically at the outer plexiform layer.
The reason why it is difficult to diagnose is that it is mostly asymptomatic and can be undetected for all of life unless it is discovered incidentally or a serious complication occurs. It was first described in 1933 by Bartels and was explored in derails in 1985 by Byer.
In most cases, it is an asymptomatic bilateral disease with a prevalence rate between 1.65% and 7.00% among individuals above 40 years of age affecting the peripheral retina in most of the cases. Acquired retinoschisis affects men and women equally and is not known to be linked genetically.
This differs from congenital retinoschisis, which is an X-linked recessively inherited vitreoretinal degeneration characterized by splitting in the nerve fiber layer typically in the fovea.
Progressive and symptomatic retinal detachment (RD) associated with Senile Retinoschisis is rare, occurring in approximately 0.05% of the cases. It is the only complication in which urgent treatment is indicated and is often difficult to conclusively differentiate between localized RD and retinoschisis using clinical observation alone.
The utility of spectral domain optical coherent tomography (SD-OCT) in successfully distinguishing retinoschisis from RD and revealing a more detailed picture of the retinal morphology has been established. This is a case of SR in the peripheral retina in which SD-OCT was utilized to report the retinal finding.
MANAGEMENT
Senile retinoschisis is usually benign but complications include:
Posterior extension or schisis cavity
The natural history is that this disease rarely progresses from where it’s first observed, so resist lasering: most cases of posterior retinoschisis will not progress beyond 3 disc diameters from the macula, and only a handful of cases of degenerative retinoschisis involving the macula have been reported.
Additionally, no treatment, including laser, has been shown to halt the progression of retinoschisis.
Although approximately three-quarters of lesions will have their most posterior extent post-equatorial, only about three percent will progress posteriorly, so most still can be observed.
Neither cataract surgery nor PVD has any adverse effect on retinoschisis because pathology is within the retina and not at the vitreoretinal interface.
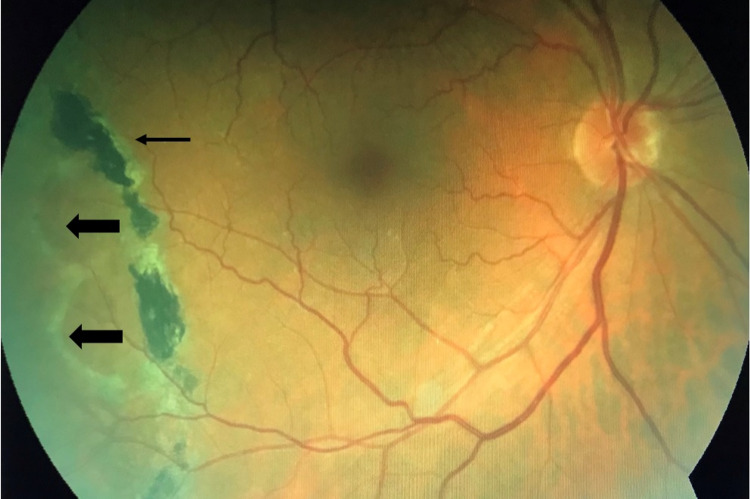
Outer wall breaks and “schisis detachment”
Outer wall breaks have a 10-27% incidence and usually can be observed. Schisis detachments may develop in a small (<10%) of eyes with schisis. This occurs when schisis fluid accumulates in the subretinal space slowly through an outer wall break.
These breaks are usually large, >3 disc diameters (DD), round, and posterior, with rolled edges. A ring of pigmentation at the border of the detachment indicates chronicity. In addition, subretinal fluid (SRF) typically doesn’t extend past the walls of schisis (viscous intraschisis fluid with mucopolysaccharides transmits slowly).
Most series notes that approximately half of RS with outer wall breaks will remain stable, and half will progress to schisis detachment. Laser demarcation or cryotherapy when the posterior margin is anterior enough has been demonstrated effective at preventing progression in the majority of patients.
Also, scatter photocoagulation to the entire bed of the schisis cavity has been noted to aid the collapse of the cavity.
One must note that although patients may be asymptomatic at the time of intervention, the decision to intervene often is due to the more posterior extent of the detachment, and retinopexy to the posterior border may introduce scotomata that may be now symptomatic for the patient.
Additionally, while rare, potential side effects of retinopexy include intraocular inflammation, retinal breaks, and epiretinal membrane formation.
Progressive rhegmatogenous retinal detachment
Progressive RRD results from breaks in both the inner and outer layers of breaks, allowing liquified vitreous to enter the subretinal space. These inner wall breaks may occur from acute PVD and vitreous traction.
However, they may be spontaneous and are often small and not easily visualized. It’s important to note that the patient may be asymptomatic due to the absolute scotoma in senile retinoschisis, even in the presence of an RRD.
However, detachments are still very rare (occur in 0.05% of patients with retinoschisis). Treatment only needs to close the inner retinal break (can leave outer retinal break).
The schisis cavity will likely recur, and it will have an absolute scotoma even if it does not. A variety of approaches have been reported with success, including laser retinopexy, cryo-retinopexy, pneumatic retinopexy, scleral buckling, and pars plana vitrectomy (PPV) with a variety of endo tamponades.
The PPVs have noted success with or without scleral buckling (SB) and with or without unroofing of the schisis cavity.
Vitrectomy is better for posteriorly located outer wall breaks and PVD, whereas SB) can be tried for anterior outer wall breaks and absence of PVD Single surgery anatomic success (SSAS) has been reported to be highest with combined SB/PPV, although given the small case rate in most series, surgery should be tailored to the patient’s presentation.
Additionally, unroofing of the schisis inner layer has been advocated to ensure complete removal of residual vitreous traction, as PVD may not be complete in many cases. No visual field impact will be had with inner layer excision as RS already results in an absolute scotoma.
The choice of approach should be guided by the location and size of the RS cavity, the number of OLH, the presence of proliferative vitreoretinopathy (PVR), and the presence of PVD.
Surgery
As above, you may consider vitrectomy or a scleral buckle in cases with retinal detachments and inner and outer retinal breaks.
However, due to the rarity of progressive schisis detachments, there is no consensus on appropriate intervention, and surgical approach varies based on the anatomy and configuration of the detachment.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Byer NE. Long-Term Natural History Study of Senile Retinoschisis with Implications for Management. Ophthalmology. 1986;93(9):1127-1137.
- Jeroudi AM, Shah V, Blinder KJ, Shah GK. Management of Degenerative Retinoschisis–Associated Retinal Detachment. Ophthalmology Retina. 2017;1(4):266-271.
- Ness S, Subramanian ML, Chen X, Siegel NH. Diagnosis and management of degenerative retinoschisis and related complications. Survey of Ophthalmology. 2022;67(4):892-907.
- Liao A, Barnett J, Rehman I, et al. Surgical Outcomes of Progressive Retinoschisis-Related Retinal Detachments: A 17-Year Survey From a Large Academic Center. Ophthalmic Surg Lasers Imaging Retina. 2022;53(3):132-138.
- Beatson B, Pham A, Ong SS, Ahmed I, Arevalo JF, Handa JT. Repair of progressive retinal detachment complicating degenerative retinoschisis: surgical management and outcomes in phakic eyes. Int J Retin Vitr. 2021;7(1):69.
- Incidence, mechanism and outcomes of schisis retinal detachments revealed through a prospective population-based study | British Journal of Ophthalmology. Accessed June 22, 2022. https://bjo.bmj.com/content/101/8/1022.long.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

