CASE REPORT
A 37-year-old male presented with a complaint of decreased vision in the right eye for 4 months. His systemic history was unremarkable. Best-corrected visual acuity (BCVA) in the right eye was 20/60 and the left eye was 20/20.
Ocular examination revealed round and normal reacting pupils with no relative afferent pupillary defect and parallel visual axes. Anterior segment examination in both eyes was unremarkable.
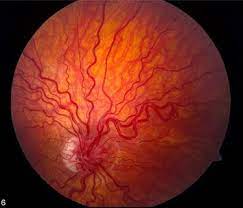
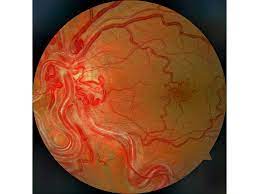
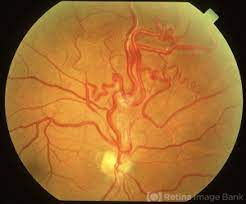
Posterior segment examination showed dilated and tortuous vessels with AV communication in both eyes with hard exudates in the macular region in the right eye. While the AVMs in the right eye were of grade II, the AVMs present in the left eye were of grade I.
The periphery was normal in both eyes. Fluorescein fundus angiography (FFA) showed normal arm-to-retina time and rapid transit time in both eyes and non-leaky retinal AV communications in the left eye, and late leakage in the perifoveal area in the right eye.
Magnetic resonance neurogram finding included tortuous vertebral arteries in close approximation with a left-side complex of cranial nerves VII and VIII and bilateral multiple tiny cavernous and capillary hemangiomas in supra- and infratentorial compartments with predominant involvement of the brainstem and cerebellum.
Hence, the patient was diagnosed with incomplete Wyburn–Mason syndrome.
Wyburn-Mason Syndrome DISEASE entity
Wyburn-Mason Syndrome (also known as Bonnet-Bechaume-Blanc syndrome, Congenital Unilateral Retinocephalic Vascular Malformation Syndrome, Racemose Angiomatosis).
Wyburn- Mason Syndrome is an exceedingly rare, non-hereditary congenital neurocutaneous disorder leading to arteriovenous malformations (AVMs).

Infants affected with Wyburn-Mason syndrome present with arteries that directly connect to veins without capillaries and lead to a fragile mass of abnormal blood vessels found in the midbrain, eyes, orbit, and rare cutaneous nevi.
Wyburn- Mason syndrome is often included in the phakomatoses syndromes, which cause tumors or masses in the brain, spinal cord, and other organs.
The exact etiology of Wyburn-Mason syndrome is currently unknown. No specific genetic or hereditary pattern has been identified.
It is hypothesized that it is caused by a sporadic abnormality in the development of blood vessels during embryonic or fetal growth. However, the exact mechanism that causes the vascular malformations is not known.
Wyburn-Mason Syndrome Diagnosis
The diagnosis of Wyburn-Mason syndrome is made with a thorough clinical exam. The dilated funduscopic exam can reveal the typical appearance of arteriovenous malformations of the retina. Brain MRI can determine the presence and extent of intracranial AVMs.
The diagnosis of the syndrome is usually delayed until late childhood because of the rarity of cutaneous manifestations.
To diagnose Wyburn-Mason, Group 3 AVMs with concomitant intracranial AVMs must be present to diagnose the syndrome. The severity and characteristics of AVMs were divided into three groups by Archer et al.
Group 1: Defined as a retinal arteriovenous malformation containing a major artery and vein with an abnormal capillary plexus in between. These lesions typically remain asymptomatic.
Group 2: Defined as a retinal arteriovenous malformation between an artery and a vein without any capillary network in between. These have a risk of retinal complications.
Group 3: Defined as complex and extensive AVMs with large vessels without a capillary plexus in between. These have a high risk for retinal complications and more likely to have intracranial
MANAGEMENT of Wyburn-Mason Syndrome
Medical Management
Traditionally, a patient with Wyburn-Mason Syndrome is followed by a cohort of physicians (ophthalmology, primary care, radiology, neurology and/or neurosurgery, and hematology), in addition to a social worker.
The majority of retinal AVM cases are stable. Treatment is reserved for patients who are visually compromised and for those who experience discomfort because of the symptoms. Management of Wyburn-Mason syndrome is conservative although surgical options are available.
Patients with retinal AVMs are recommended to have brain imaging to rule out intracranial AVMs. Regular ophthalmologic evaluations are required to monitor AVMs and their potential complications.
Surgical Management
Certain brain AVMs, depending on location, can be surgically resected. For AVMs that are not amenable to surgery, alternative measures, such as embolization and radiation therapy, may be considered.
Radiation therapy, such as Linac, Gamma knife, Cyberknife, and embolization, which is a catheter technique that delivers an occlusive substance to the abnormal vessel can be considered. Embolization of AVMs is performed by neuroradiologists or neurosurgeons.
Complications of retinal AVMs including neovascularization of the retina into the vitreous or neovascular glaucoma from retinal vein occlusions can be treated with pan-retinal photocoagulation and consideration of anti-angiogenic agents.
Macular edema secondary to vein occlusions can also be treated with intravitreal anti-VEGF agents. Pars plana vitrectomy can be considered for massive vitreous hemorrhage that does not clear after a few weeks. Another indication for pars plana vitrectomy includes traction retinal detachments.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Kaplan, Henry J. “Wyburn Mason Syndrome.” Retina Image Bank, 2013, imagebank.asrs.org/file/6211/wyburn-mason-syndrome.
- So JM, Holman RE. Wyburn-Mason Syndrome. [Updated 2020 Feb 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.
- Schmidt D, Pache M, Schumacher M. The congenital unilateral retinocephalic vascular malformation syndrome (Bonnet-Dechaume-Blanc syndrome or Wyburn-Mason syndrome): a review of the literature. Surv Ophthalmol. 2008;53:227-49.
- Liu W, Sharma S. Ophthaproblem. Retinal arteriovenous malformations (type 2). Can Fam Physician. 2005;51(2):203–209.
- Miller, Neil R., et al. Walsh and Hoyt’s Clinical Neuro-Ophthalmology. Williams & Wilkins, 1998.
- Rao P, Thomas BJ, Yonekawa Y, Robinson J, Capone A, Jr. Peripheral retinal ischemia, neovascularization, and choroidal infarction in wyburn-mason syndrome. JAMA Ophthalmol 2015;133:852-54.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

