CASE REPORT
A 52-year-old male presented visual acuity loss of his right eye (OD) 2 days after an uncomplicated ranibizumab IVI with a 30G needle.
The past medical history included PE, high myopia, and OD pars plana vitrectomy due to retinal detachment. He was being treated with monthly ranibizumab due to choroidal neovascularization secondary to angioid streaks, with 78 previous injections in the OD.
At presentation, his BCVA was 6/18 and the intraocular pressure (IOP) was 3 mmHg. Slit-lamp examination of the anterior segment was unremarkable.
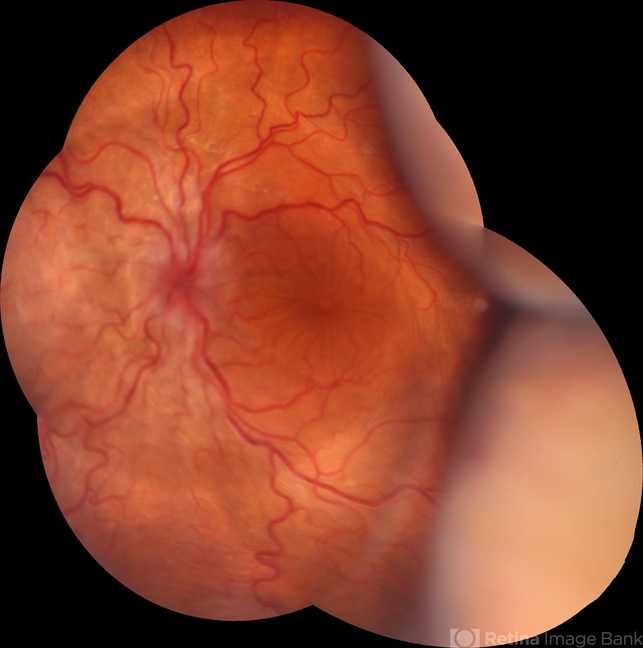
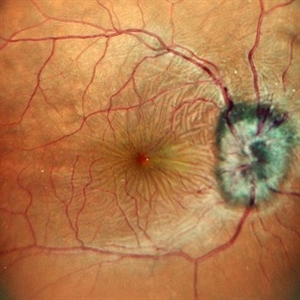
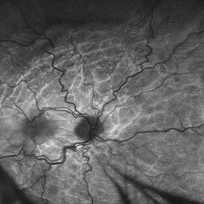
Smartphone Fundoscopy and OCT scans revealed posterior pole chorioretinal folds. Altogether, the low intraocular pressure and fundoscopic findings led to the diagnosis of hypotony maculopathy.
Hypotony Maculopathy DISEASE entity
Hypotony maculopathy may be defined both statistically and clinically. The statistical definition of hypotony is intraocular pressure (IOP) less than 6.5mmHg, which is more than 3 standard deviations below the mean IOP.
The clinical definition of hypotony maculopathy is IOP low enough to result in vision loss. The vision loss from low IOP may be caused by corneal edema, astigmatism, cystoid macular edema, or maculopathy.
Hypotony maculopathy is characterized by a low IOP associated with fundus abnormalities, including chorioretinal folds, optic nerve head edema in the acute setting, and vascular tortuosity.
It may occur after ocular inflammation, trauma, or surgery. Most cases are secondary to glaucoma filtration surgery with a reported incidence of 1.3% to 18%. Furthermore, the risk of hypotony maculopathy increases with the use of antifibrosis agents during glaucoma surgery.
Postoperative Hypotony
- Mitomycin C (MMC) toxicity of the ciliary body
- Over filtration
- Bleb Leak
- Wound Leak
- Iridocyclitis
- Cyclodialysis
- Ciliochoroidal Detachment
- Retinal Detachment
Traumatic Hypotony
- Scleral perforation
- Retinal Detachment
- Cyclodialysis
- Iridocyclitis
- Ciliochoroidal Detachment
Bilateral Hypotony
- Osmotic Dehydration
- Diabetic coma
- Uremia
- Myotonic Dystrophy
Miscellaneous forms of hypotony
- Ciliary body hypoperfusion from vascular occlusive disease
Hypotony Maculopathy MANAGEMENT
Medical and Conservative Management:
The successful treatment of hypotony maculopathy depends on the identification of the underlying etiology and its appropriate treatment. The most common cause of hypotony maculopathy is recent glaucoma filtration surgery that may result in either a bleb leak or an over-filtering bleb.
In the case of a bleb leak, conservative measures include aqueous suppressants, topical antibiotics, or the use of a bandage contact lens. Aqueous suppressants reduce the aqueous outflow through the leak which may facilitate healing of the overlying epithelium.
A bandage contact lens promotes epithelial migration and wound healing. A topical antibiotic provides prophylaxis for infection. Aminoglycosides may induce conjunctival inflammation that can stimulate wound healing.
Cyanoacrylate glue, autologous blood injection, and compression sutures are other options that can be employed.
Various treatment strategies for an over-filtering bleb include a quick tapering regimen of topical steroids, autologous blood injection, use of a laser to stimulate inflammation, diathermy, trichloroacetic acid, and compression sutures to minimize aqueous outflow.

In case hypotony is due to uveitis and hyposecretion, corticosteroids are given to reduce inflammation and thus improve ciliary body function. Inflammation reduces aqueous production and increases uveoscleral outflow. Topical cycloplegics are also used to relax the iris and ciliary body, reducing the potential space for subsidiary effusions.
Surgical Management:
Surgical intervention is undertaken immediately in cases of trauma, including scleral rupture or retinal detachment. In other etiologies, conservative management should be utilized first, as described above.
If these measures fail to resolve the hypotony maculopathy, surgical intervention is warranted. Bleb excision and revision may be required using either the conjunctival advancement approach or a free conjunctival autograft.
Vitrectomy has also been described as a method of a possible treatment for unresolving chorioretinal folds. An ILM peel may provide the elimination of contractile forces from subclinical fibrocellular proliferation.
Perfluorocarbon liquid has been described as a “steam-roller” of the retina flat by temporarily increasing the intraoperative IOP to 50 mm Hg intraoperatively.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- American Academy of Ophthalmology. Hypotony maculopathy.
- Gass JD. Hypotony maculopathy. In: Bellows JG (ed.) Contemporary ophthalmology. Honoring Sir Stewart Duke-Elder. Baltimore: Williams & Wilkins. 1972:343–366.
- Costa VP, Arceiri ES.Hypotony maculopathy. Acta Ophthalmol 2007;586-597.
- Fannin LA, Schiffman JC, Budenz DL.Risk factors for hypotony maculopathy. Ophthalmology. Jun 2003;110(6):1185-91.
- Minckler DS, Bunt AH.Axoplasmic transport in ocular hypotony and papilledema in the monkey. Arch.Ophthalmol 95:1430-1436.
- Budenz DL, Schwartz K, Gedde SJ.Occult hypotony maculopathy diagnosed with optical coherence tomography. Arch Ophthalmol 2005;123:113-114.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE



I really appreciate your help
May I request more information on the subject? All of your articles are extremely useful to me. Thank you!
Thank you for writing this article. I appreciate the subject too.