CASE REPORT
A 29-year-old woman presented with a chief complaint of experiencing acute onset paracentral visual field defect from 5 days ago in the left eye.
She had a positive SARS-CoV-2 reverse transcription-polymerase chain reaction (RT-PCR) test in past medical history, performed following fever, headache, and non-productive cough 2 weeks before the beginning of ocular symptoms.
The symptom was mild, so the patient was advised to self-quarantine without receiving any specific medication. The mild respiratory symptoms were relieved by the use of paracetamol and diphenhydramine.
Previous ocular, medical, and family histories were unremarkable except for COVID-19. She had no prior history of medication consumption, sun-gazing, or eye trauma.
Ophthalmological examination revealed equally round and reactive to light and accommodation pupils with normal slit-lam bio-microscopy. Intraocular pressure was normal.
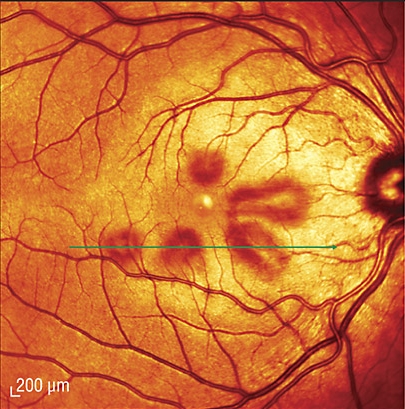
The fundoscopic evaluation demonstrated a sharply contoured and well-perfused disc as well as a yellow spot in the fundus left eye.
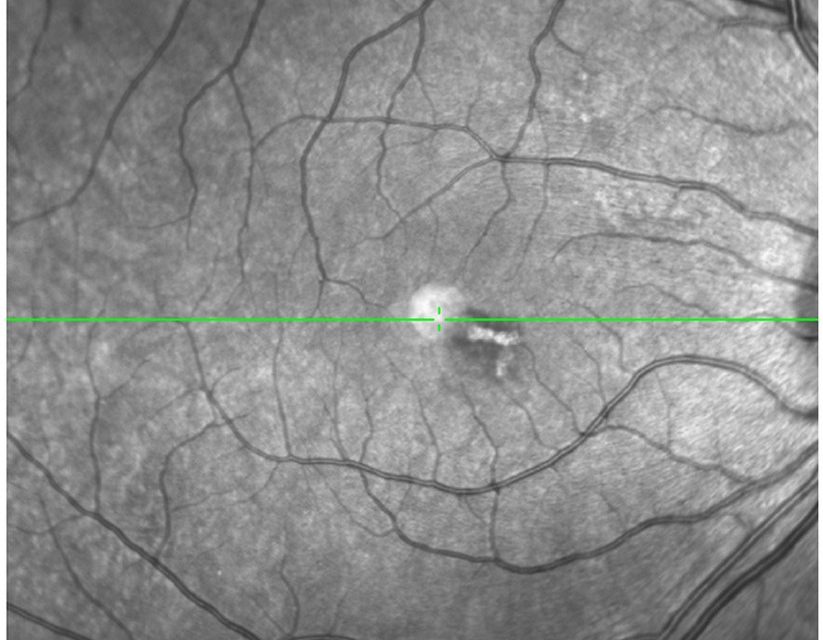
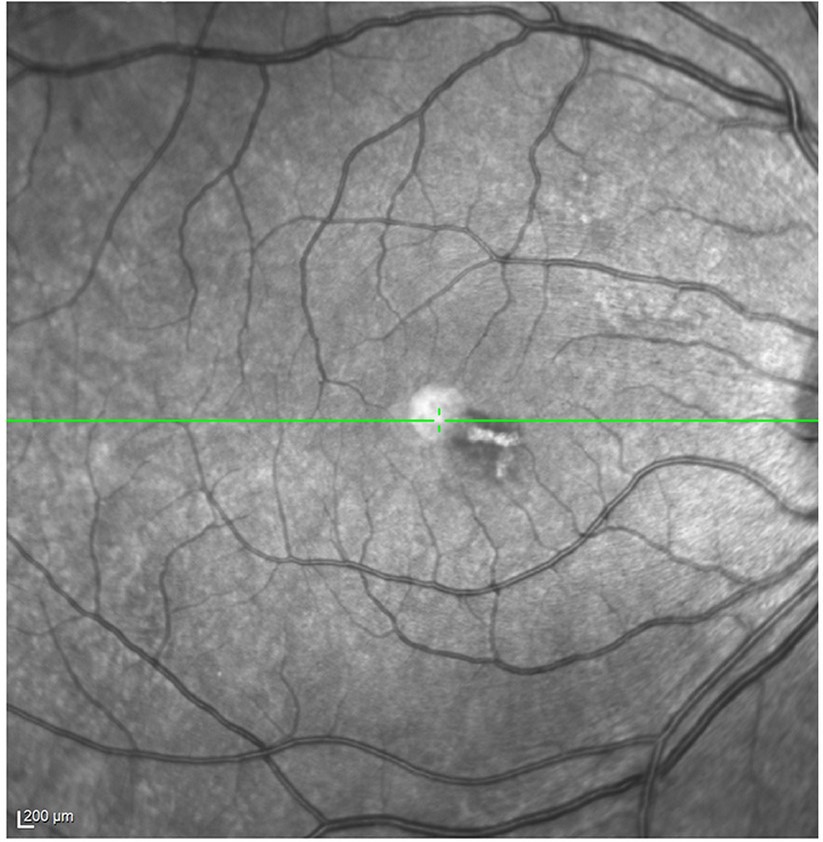
Infrared imaging revealed a subtle, grayish wedge-shaped lesion surrounding the fovea compatible with the hypo-reflective area in the left eye.
Additionally, spectral-domain optical coherence tomography (SD-OCT) demonstrated the disruption of the inner segment/outer segment junction (ellipsoid zone).
Based on the patient’s history and ocular assessments, a diagnosis of Acute Macular Neuroretinopathy (AMN) was confirmed.
Acute Macular Neuroretinopathy DISEASE entity
Acute Macular Neuroretinopathy (AMN), first reported in 1975 (by Bos and Deutman), is a rare disease, commonly affecting young women, that causes transient or permanent vision loss. AMN is defined by the presence of intra-retinal, reddish-brown, wedge-shaped lesions around the fovea.
Patients with AMN report a sudden onset of one or more paracentral scotomas, decreased vision, and/or blurry vision.
Scotomas generally persist indefinitely, though some resolve partially over months. In the majority of patients, the fovea is spared; however, prior studies have found patients with foveal involvement, including foveal hemorrhage, foveal granularity, and abnormal foveal reflex.
Although exact mechanisms causing Acute Macular Neuroretinopathy (AMN) have yet to be elucidated, there is evidence to suggest that vascular compromise of the deep retinal capillary plexus of the retina leads to vision loss seen in patients with this disease.
Another theory has been postulated regarding systemic inflammation in autoimmune diseases causing microthrombosis due to small-vessel occlusion, thus leading to ischemic retinopathy.
Acute Macular Neuroretinopathy Diagnostic Procedures and Tests
Funduscopic examination is often initially normal. Typically, lesions become visible 3 days to 2 months after symptom onset. Classically, retinal lesions involve one or more reddish-brown, petalloid lesions that surround the fovea.
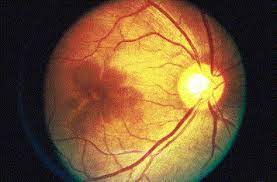
Such lesions can be subtle clinically and may be better seen with red-free light. These lesions correspond closely to Amsler grid findings of the scotoma. Faint intraretinal hemorrhages can be seen.
The imaging modalities most commonly used to evaluate the lesion(s) are:
1. Infraredfundusphotography. SD-Optical Coherence Tomography (OCT) machines use infrared light to illuminate the macula for the photographer prior to any cross-sectional images being obtained. Lesions are visible as dark gray, petalloid, perifoveal lesions with the tip pointed toward the fovea.
These correspond anatomically to the scotomas if the patient draws them on an Amsler grid or if they are documented via formal visual field testing.
2. SD-OCT: Hyperreflective plaque is seen initially at the outer nuclear (ONL) and outer plexiform layers of OCT, indicating disruption of photoreceptor cell bodies and their axons.
Focal ellipsoid zone (EZ) disruption ensues. With time, EZ reconstitutes but persistent interdigitation zone disruption is noted. The hyper-reflective plaque fades away and is replaced with ONL thinning.
3. OCT-A reveals reduced flow signals in deep retinal capillary plexus, suggesting focal ischemia photoreceptor axons in the outer plexiform layer.
Variable recovery of capillary flow signal is noted with time in the deep capillary plexus. However, the entire damaged photoreceptor unit atrophies causing cumulative long-term ONL thinning.
4. Fluorescein angiography is noted to be normal in most cases. Subtle hypofluorescence of the lesions may be noted early and late phases of the study.
5. Adaptive Optics shows reduced cone photoreceptor density and cone mosaic disruption with incomplete recovery with time.
6. Multifocal ERG reveals diminished amplitudes in most eyes and, occasionally, decreased implicit time may also be noted.
Acute Macular Neuroretinopathy MANAGEMENT
No medication has been shown to improve the condition. Even though there are rare associations between hormonal contraceptive use and excessive coffee consumption, there is no recommendation in the literature that patients should discontinue these if they develop this disease.

Follow-up is at the discretion and comfort level of the physician. If the diagnosis is considered relatively certain based on history and the presence of classic findings, then follow-up maybe every few weeks or months simply to document the course of the disease. No intervention can be performed for this disease.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Bos PJ, Deutman AF. Acute macular neuroretinopathy. Am J Ophthalmol. 1975;80(4): 573-84.
- Rennie AT, DeWeerd AJ, Martinez MG, Kay CN. Acute Macular Neuroretinopathy Following COVID-19 mRNA Vaccination. Cureus. 2022 Jul 31;14(7):e27502. doi: 10.7759/cureus.27502. PMID: 36060339; PMCID: PMC9426360
- Rahimy, E, & Sarraf, D. (2014). Paracentral acute middle maculopathy spectral-domain optical coherence tomography feature of deep capillary ischemia. Curr Opin Ophthalmol, 25(3), 207-212. doi:10.1097/icu.0000000000000045.
- Bhavsar KV, Lin S, Rahimy E, Joseph A, Freund KB, Sarraf D, Cunningham ET Jr. Acute macular neuroretinopathy: A comprehensive review of the literature. Surv Ophthalmol. 2016;61(5):538-65.
- Acute macular neuroretinopathy: pathogenetic insights from optical coherence tomography angiography. Casalino G, Arrigo A, Romano F, Munk MR, Bandello F, Parodi MB. Br J Ophthalmol. 2019;103:410–414.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE