CASE REPORT
A 30 years old male presented with complaints of blurred vision and photophobia since birth, accompanied by a family history of similar eye conditions.

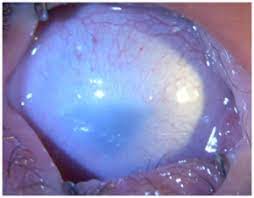
A comprehensive ophthalmic examination revealed significantly reduced visual acuity, Slitlamp examination findings, and corneas that appeared opaque and hazy with a loss of normal transparency, poorly demarcated limbal area, absence of neovascularization, and normal intraocular pressure.
A diagnosis of Sclerocornea was made based on these clinical findings.
Sclerocornea: DISEASE entity
Sclerocornea is a rare, non-progressive, bilateral, and asymmetric primary congenital disease that has no association with inflammatory and/or infectious causes.

Sclerocornea is defined as diffuse (total) or peripheral opacity of the cornea, either associated or not with the flat cornea and systemic changes (mental retardation, deafness, and craniofacial abnormalities).
There is no sex predilection. The opacity of the cornea is similar to the sclera, white and vascularized, with no delimitation of the limbus, making it difficult to assess the corneal diameter correctly in cases of peripheral involvement, the central region shows up with variable transparency.
Initially, Waring et al. proposed a classification of sclerocornea:
- Isolated peripheral sclerocornea: sclerotization of the cornea, with no other associated anomalies.
- Plana Sclerocornea: flat cornea associated with keratometry < 38D, leading to high hyperopia.
- Sclerocornea associated with anterior chamber alterations: the presence of anterior segment anomalies, such as iridocorneal adhesions.
- Total sclerocornea: diffuse opacity.
Sclerocornea MANAGEMENT
Patients with sclerocornea or any congenital opacity must be submitted to ophthalmological assessment and complementary exams to exclude other associated eye diseases such as glaucoma.
It is necessary to carry out a systemic and genetic assessment in search of associated diseases, in addition to genetic counseling. On the whole, the treatment of congenital corneal opacities that affect the visual axis is surgical, with penetrating keratoplasty being used as the method of choice.
Besides that, in order to avoid the development of deprivation amblyopia the surgery must be performed as early as possible. It is known that the visual prognosis in patients diagnosed with sclerocornea is poor and there is high rates of graft rejection in the 5-year follow-up.
Kim et al showed failure in 75% of the cases of PK (penetrating keratoplasty) in patients with sclerocornea. The factor associated with graft failure was vascularization in the limbal region or in the periphery of the cornea. Other factors such as secondary glaucoma and the presence of iridocorneal adhesions were not identified as risk factors.
In the largest series of patients with a total (15 eyes) and partial (12 eyes) sclerocornea clinically diagnosed and undergoing penetrating keratoplasty, Frueh and Brown found 70% graft survival in the 1-year follow-up.
In the series by Michaeli et al, six children with sclerocornea and 12 operated eyes, only 37% of the grafts remained clear in the 1-year follow-up. The poor prognosis of corneal transplantation in sclerocornea is related to corneal vascularization, associated ocular changes, mainly glaucoma, and the need for concomitant surgeries such as lensectomy and vitrectomy, among others.

In patients with partial sclerocornea and free visual axis, optical correction, with glasses, should be performed early in order to avoid amblyopia due to high hyperopia.
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Nischal, K.K., Genetics of Congenital Corneal Opacification–Impact on Diagnosis and Treatment. Cornea, 2015. 34 Suppl 10: p. S24-34.
- Mark J. Mannis MD FACS, E.J.H.M., Cornea. 4th ed. 2017, China: Elsevier.
- Aldave, A.J., et al., Autosomal dominant cornea plana are not associated with pathogenic mutations in DCN, DSPG3, FOXC1, KERA, LUM, or PITX2. Ophthalmic Genet, 2007. 28(2): p. 57-67.
- Mataftsi, A., et al., Chromosome abnormalities and the genetics of congenital corneal opacification. Mol Vis, 2011. 17: p. 1624-40.
- Quiroz-Casian, N., et al., Sclerocornea-Microphthalmia-Aphakia Complex: Description of Two Additional Cases Associated With Novel FOXE3 Mutations and Review of the Literature. Cornea, 2018. 37(9): p. 1178-1181.
- Nischal, K.K., Congenital corneal opacities – a surgical approach to nomenclature and classification. Eye (Lond), 2007. 21(10): p. 1326-37.
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE


I enjoyed reading your piece and it provided me with a lot of value.