CASE REPORT
ِِA 25-year-old man was referred to an ophthalmology clinic due to vision loss in his left eye. He has no past medical or ocular history, and he is not taking any medications. Additionally, he is a non-smoker and drinks alcohol socially.
The patient reported waking up with vision loss in his left eye five days ago and sought medical attention at an urgent care center, where he was then referred to ophthalmology. He denies experiencing eye pain or pain with eye movements but has been feeling fatigued, and tired, and developed a low-grade fever over the past few days.
During the ophthalmological examination, his visual acuity was 20/20 in the right eye, and counting fingers in the left eye. Pupils were equal, but a left relative afferent pupillary defect (RAPD) was observed.
Color vision using Ishihara color plates was normal in the right eye (14/14) but impaired in the left eye (0/14). Ocular motility and alignment were found to be normal, and the slit lamp examination did not reveal any abnormalities. However, the left eye exhibited 1/2+ cells in the vitreous.
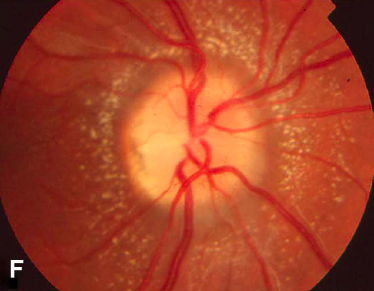
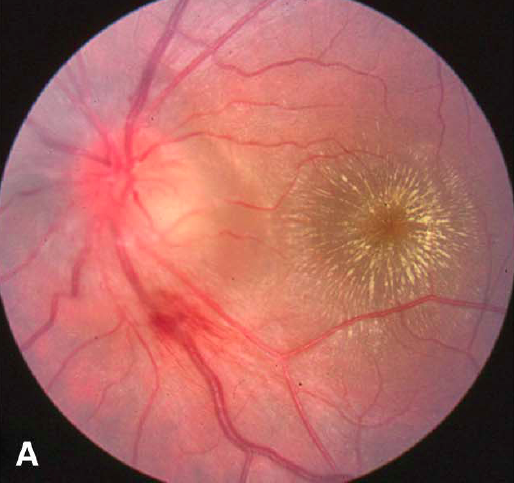
The neurological examination yielded normal results. Despite these findings, the patient’s examination is considered atypical for neuroretinitis due to the significant optic disc edema and subretinal fluid in the macula observed in the left eye.
ًWhat is Neuroretinitis?
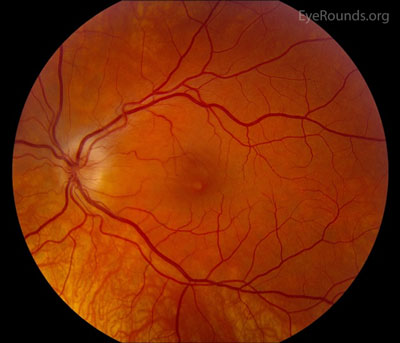
Neuroretinitis is an inflammation of the neural retina and optic nerve. It was originally described by Leber in 1916 as a “stellate maculopathy,” but this definition was challenged by Don Gass in 1977, citing that disc edema precedes macular exudates.

Subsequently, Gass confirmed optic disc leakage by fluorescein angiography and suggested the term “neuroretinitis.” More recent retinal and optic nerve imaging has supported Gass’ description.
Risk factors for neuroretinitis relate to susceptibility to each particular causative agent. Immunocompromised patients from chronic disease, HIV/AIDS, medications, health care workers, recent immigrants, or those with recent travel to endemic areas are all high-risk populations.
Neuroretinitis MANAGEMENT
General treatment
The treatment of neuroretinitis is directed at the underlying etiology. Suspicion for infectious etiology, particularly tuberculosis, may merit consultation with an infectious disease specialist.
If the causative agent is found to be cat-scratch disease, various treatment methods are found in the literature, including no treatment, antibiotics only, antibiotics and steroids, and steroids only.
As a high degree of spontaneous visual recovery exists in cat-scratch disease neuroretinitis, definite conclusions cannot be made regarding antibiotic efficacy.
If an infectious etiology is suspected, an appropriate workup with broad-spectrum antibiotic treatment, while results are pending, is appropriate. Recommended antibiotics are ciprofloxacin or azithromycin for adults and azithromycin or sulfamethoxazole-trimethoprim for children.
For the idiopathic variety, high-dose oral corticosteroids have been administered. Antibiotics may be considered to cover cat-scratch disease while serologies are pending.
Medical follow up
If an infectious etiology is suspected but serologies are negative, retesting at six weeks for rising IgG titers is appropriate.
Neuroretinitis Complications
Complications stem from side effects from pharmacologic therapy or chronic visual loss from recurrence. Anti-tuberculous treatments are well-known for ocular complications, including retrobulbar neuritis with ethambutol and significant anterior uveitis, and hypopyon with rifabutin therapy.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Fouch B, Coventry S. A case of fatal disseminated Bartonella henselae infection (cat-scratch disease) with encephalitis. Arch Pathol Lab Med. 2007;131(10):1591-4.
- Ghauri R, Lee A. Optic Disk Edema With a Macular Star. Survey of Ophthalmology. 43(3): 270-4, 1998.
- Purvin VA, Chioran G. Recurrent neuroretinitis. Arch Ophthalmol. 1994;112:365-71.
- Purvin V, Sundaram S, Kawasaki A. Neuroretinitis: Review of the Literature and New Observations. J Neuro-Ophthalmology. 2011;31: 58-68.
- Vaphiades MS. Rocky Mountain Spotted Fever as a cause of macular star figure. Neuroophthalmol. 2003;23(4):276-8.
- Vaphiades MS, Wigton EH, Ameri H, Lee AG. Neuroretinitis with retrobulbar involvement. J Neuroophthalmol. 2011;31(1):12-5.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

