CASE REPORT
A 7-year-old healthy boy was referred to the uveitis clinic because of bilateral uveitis discovered on a routine eye exam. On presentation, he was treated with prednisone (25 mg/day).
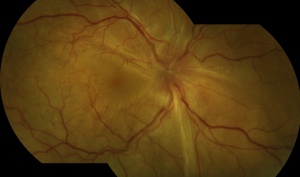
On examination, visual acuity (VA) in the right eye (RE) was 6/9 and in the left eye (LE) was 6/15. Near vision was RE J1 + and LE J7. The anterior segments were normal. Fundoscopy revealed bilateral vitritis, snowballs, and bilateral inferior retinoschisis.
Spectral-domain optical coherence tomography (SD-OCT) showed normal foveal contour bilaterally. There was no subjective or objective evidence of an underlying disease.
Systemic work-up including complete blood count, erythrocyte sedimentation rate, C-reactive protein, Angiotensin-converting enzyme, liver, and kidney function tests, chest x-ray, and serology for Syphilis, Toxoplasma, and Toxocara was un-yielding.
The child was diagnosed as having PP-associated inferior retinoschisis. Oral methotrexate was introduced as a steroid-sparing agent and prednisone tapered. Two months later, the RE retinoschisis was resolved.
Five months later, RE VA was 6/7.5 and LE VA was 6/12 and near vision was J1 in each eye. Subsequently, the child was lost to follow-up and presented 3 years later with LE drop in the vision of 3 week-duration. During these years the parents of the patient discontinued methotrexate.
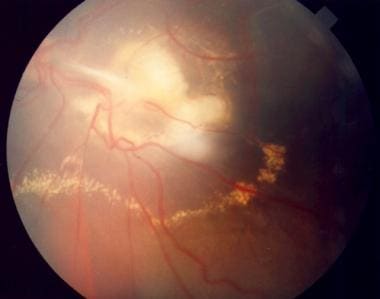
On examination, RE VA was 6/7.5, and LE VA was 6/60. Near vision was RE J1, LE J16. RE fundoscopy revealed snowballs inferiorly. LE biomicroscopy showed active anterior-uveitis. LE fundoscopy revealed total RD. No retinal breaks or tractional membranes were seen and no choroidal detachment.
Fluorescein angiography revealed profuse vascular leakage all over the left fundus with intense leakage in the nasal and temporal periphery. SD-OCT showed left macular detachment with intra and subretinal fluid.
The child was diagnosed with total Exudative Retinal Detachment (RPE)
Exudative Retinal Detachment DISEASE entity
Exudative (or serous) retinal detachment (ERD) occurs when fluid accumulates in the subretinal space between the sensory retina and the retinal pigmented epithelium (RPE) resulting in retinal detachment. Causes for fluid accumulation include inflammatory, infectious, and neoplastic diseases of the choroid or retina.

The subretinal space, a remnant of the embryonic optic vesicle, is practically nonexistent in a healthy eye. However, pathologies that disrupt the integrity of the blood-retina barrier (BRB) can cause leakage of fluid that enlarges the subretinal space and separates the sensory retina from the RPE resulting in retinal detachment.
The BRB has an inner and outer component. The inner blood-retina barrier (iBRB) is composed of tight junctions in between cells of the retinal endothelium whereas the outer blood-retina barrier (oBRB) is composed of tight junctions between cells of the Exudative Retinal Detachment (RPE).
MANAGEMENT of Exudative Retinal Detachment
Treatment
Unlike rhegmatogenous and tractional detachments which are treated surgically, ERD is generally treated medically. Treatment focuses on the underlying pathology causing the fluid buildup.

Medical
Immunosuppressive
For ERD caused by non-infectious uveitis (e.g. VKH syndrome), the common treatment is high-dose IV steroids followed by oral steroid taper. Intravitreal triamcinolone has also been used. Alternatives to steroids include cyclosporine A, azathioprine, methotrexate, mycophenolate mofetil, and infliximab.
Biologics
Tumor necrosis factor (TNF) alpha inhibitors (etanercept, infliximab, adalimumab), interferon alpha-2, interferon-beta, specific cell inhibitors (rituximab, daclizumab) and receptors antagonists (anakinra, efalizumab).
Anti-VEGF
Intravitreal bevacizumab (IVB) can be helpful for subretinal fluid exudation due to its anti-angiogenic and anti-permeability properties.
Other
Eplerenone (mineralocorticoid receptor antagonist) for CSC.
Interventional
Focal laser photocoagulation, cryotherapy, low-dose plaque radiotherapy, photodynamic therapy (PDT), and pars plana vitrectomy (PPV).
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Amer R, Nalcı H, Yalçındağ N, Exudative Retinal Detachment, Survey of Ophthalmology (2017), doi: 10.1016/j.survophthal.2017.05.001.
- Blair K, Czyz CN. Retinal Detachment. [Updated 2021 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551502/
- Cunha-Vaz J, Bernardes R, Lobo C. Blood-retinal barrier. Eur J Ophthalmol. 2011;21 Suppl 6:S3-9. doi: 10.5301/EJO.2010.6049. PMID: 23264323.
- Fineman, M. S., & Ho, A. C. (2012). Color Atlas & Synopsis of Clinical Ophthalmology: Retina. Lippincott Williams & Wilkins.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE


Your articles are extremely helpful to me. May I ask for more information?