CASE REPORT
A 30-year-old female with recent ankle surgery presented to an ophthalmology eye center with decreased visual acuity in her right eye and complained of a “black spot” in her central vision that occurred 2 weeks prior after she had surgery done on her ankle.
She wears single-vision distance glasses with no previous eye surgery and no eye or head trauma. The visual disturbance was constant and gradually worsening. Her Best Corrected Visual Acuity (BCVA) was 20/40 in the right eye and 20/20 in the left eye.
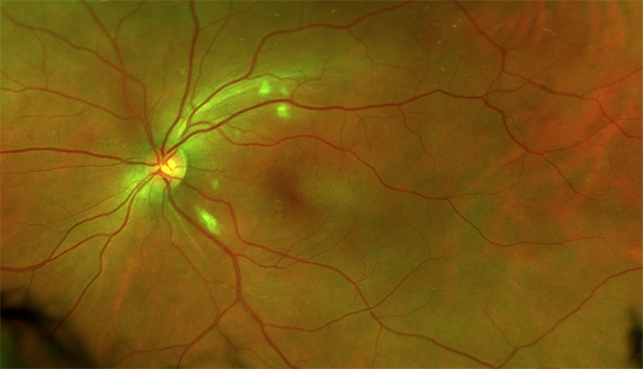
The Intraocular Pressures (IOP) obtained by the iCare tonometer were 16 on the right and 17 on the left. Fundus examination of the left eye showed a normal anterior segment and subtle swelling of the optic disc. The right eye had an inferior corneal scar and severe swelling of the optic disc with Paton’s lines or retinal folds indicative of papilledema.
Fundus examination of the right eye also showed mild edema of the macula and scattered white dots and discoloration of the retina. The patient was referred to a retina specialist for further evaluation the next day. Her visual acuity the following day was 20/25-1 on the right and 20/20 on the left.
The IOP obtained by Tono-Pen was 12 on the right and 13 on the left. An Optic Coherence Tomography (OCT) was ordered and the findings showed retinal thickening consistent with macula edema in both eyes.
Given the patient’s history of retinal findings, she was diagnosed with Purtscher retinopathy in both eyes (the right side is worse than the left).
Purtscher Retinopathy DISEASE entity
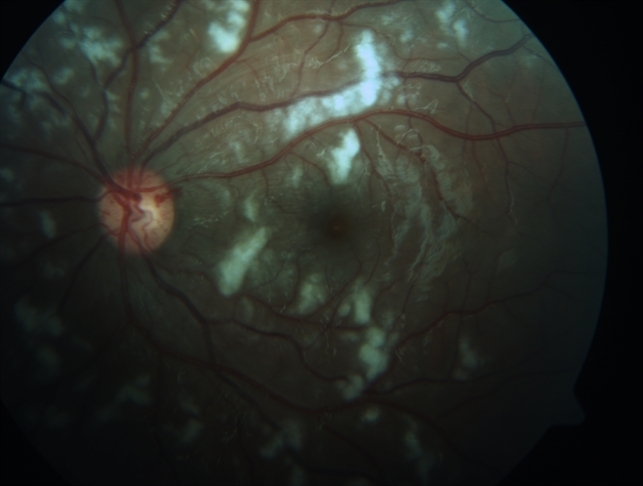
Purtscher retinopathy (traumatic retinal angiopathy or lymphorrhagia retinae or retinal teletraumatism) is an occlusive micro vasculopathy characterized by multiple retinal white areas around the optic nerve head and fovea with perivascular clearing, which may be associated with intraretinal hemorrhages.
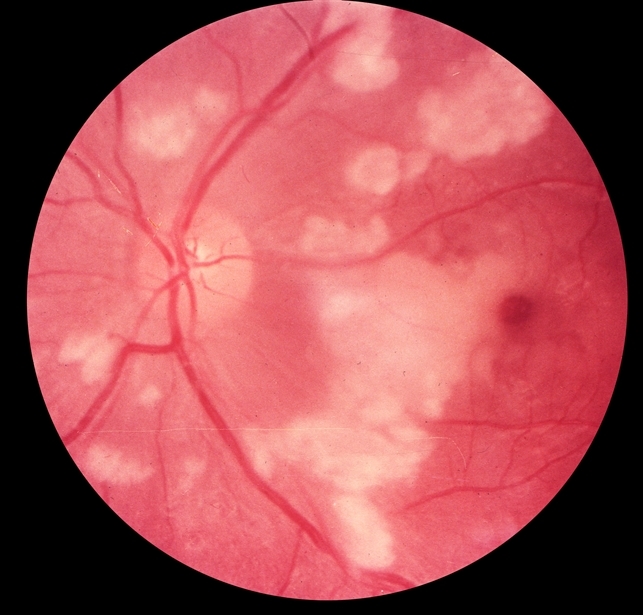
Purtscher flecken, cotton wool spots, and minimal intraretinal hemorrhage are typical features. Management depends on the cause and the role of systemic steroid need further evaluation. Typical Purtscher retinopathy described by Otmar Purtscher has features like severe visual decline after head trauma.
In the initial report, it was noted to be associated with multiple superficial retinal white patches, retinal hemorrhages, and optic disc edema.
Purtscher retinopathy is associated with trauma/surgery. The causes include:
- Severe head trauma
- Chest compression
- Fracture of long bones (e.g., femur) or crush injury
- Dislocation of the shoulder joint and avulsion fracture of the greater tuberosity of the humerus
- Barotrauma
- Battered baby syndrome
Purtscher Retinopathy MANAGEMENT
The management of Purtscher retinopathy consists of managing the cause and supportive therapy. A systematic review did not find any difference in the improvement of visual acuity when they compared treatment with steroids versus observation.
However, there are reports of visual and anatomical improvement with three daily doses of intravenous methylprednisolone pulse (1000mg) followed by oral steroids. The proposed mechanism of action includes stabilization of the microvasculature and neuronal membrane and inhibition of granulocyte aggregation.
Cases with macular edema may benefit from anti-vascular endothelial growth factor agents like bevacizumab. Lupus retinopathy, a common differential for Purtscher-like retinopathy, signifies systemic activity of systemic lupus erythematosus. Such cases require systemic steroids (oral with or without intravenous pulse methylprednisolone) and immunosuppression.
A case of the atypical hemolytic uremic syndrome with thrombotic microangiopathy and Purtscher-like retinopathy had successful treatment with eculizumab (a monoclonal antibody that inhibits cleavage of C5 to C5a and C5b, thereby blocking the terminal pathway of the complement system).

Other therapies attempted for this retinopathy include oral nonsteroidal anti-inflammatory drugs (indomethacin) and papaverine hydrochloride. Future research is needed to manage thrombotic microangiopathy, which is a crucial factor in the pathogenesis of many cases. Bortezomib, a proteasome inhibitor, can deplete the ADAMTS-13 antibody (which plays a vital role in thrombotic microangiopathy) in TTP.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Roncone DP. Purtscher’s retinopathy. Optometry. 2002 Mar;73(3):166-72.
- Miguel AI, Henriques F, Azevedo LF, Loureiro AJ, Maberley DA. A systematic review of Purtscher’s and Purtscher-like retinopathies. Eye (Lond). 2013 Jan;27(1):1-13.
- Xia D, Chen X, Zhou Q, Xiao S, Yu Y, Wang Y, Du G, Huang H, Zhang W, Chen Y. Efficacy of Purtscher’s Retinopathy Treatments: A Systematic Review. Curr Eye Res. 2017 Jun;42(6):908-917.
- Agrawal A, McKibbin M. Purtscher’s retinopathy: epidemiology, clinical features, and outcome. Br J Ophthalmol. 2007 Nov;91(11):1456-9.
- Nayak H, Harun S, Palimar P. Purtscher’s retinopathy after fracture dislocation of the shoulder joint. Emerg Med J. 2005 Nov;22(11):831-2.
- Demazure S, Gogneaux L, Ansquin M. [Post-traumatic Purtscher’s retinopathy caused by chest compression following a motor vehicle accident: A case report]. J Fr Ophtalmol. 2021 Nov;44(9):e563-e565.
- Ortmaier R, Resch H, Stieböck C, Stundner O, Arlt EM. Purtscher’s retinopathy after intramedullary nailing of a femoral shaft fracture in a 20-year-old healthy female – report of a rare case and review of the literature. BMC Musculoskelet Disord. 2014 Feb 19;15:42.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE


The articles you write help me a lot and I like the topic