CASE REPORT
A 10-year-old boy presented with a bilateral decreased vision since the age of three. His parents were consanguineous but normal on ophthalmic examinations. Best-corrected visual acuity (BCVA) was 20/160 and 20/800 in his right and left eyes with corrections of −12.00 and −13.00 sphere, respectively.
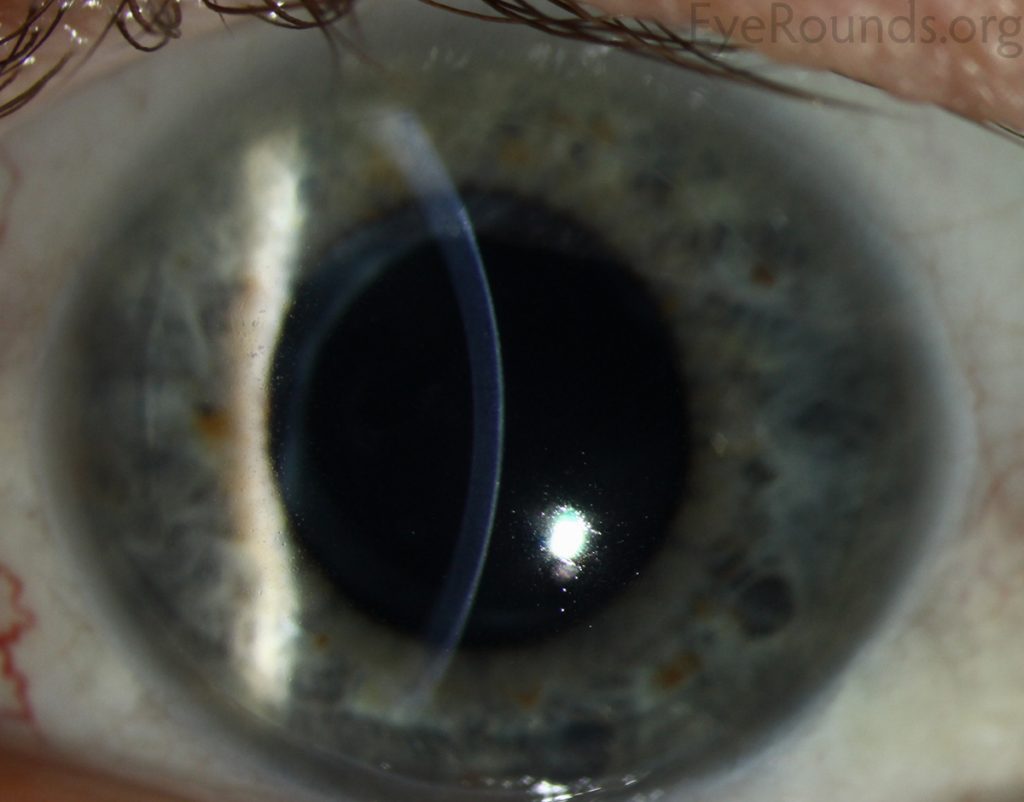
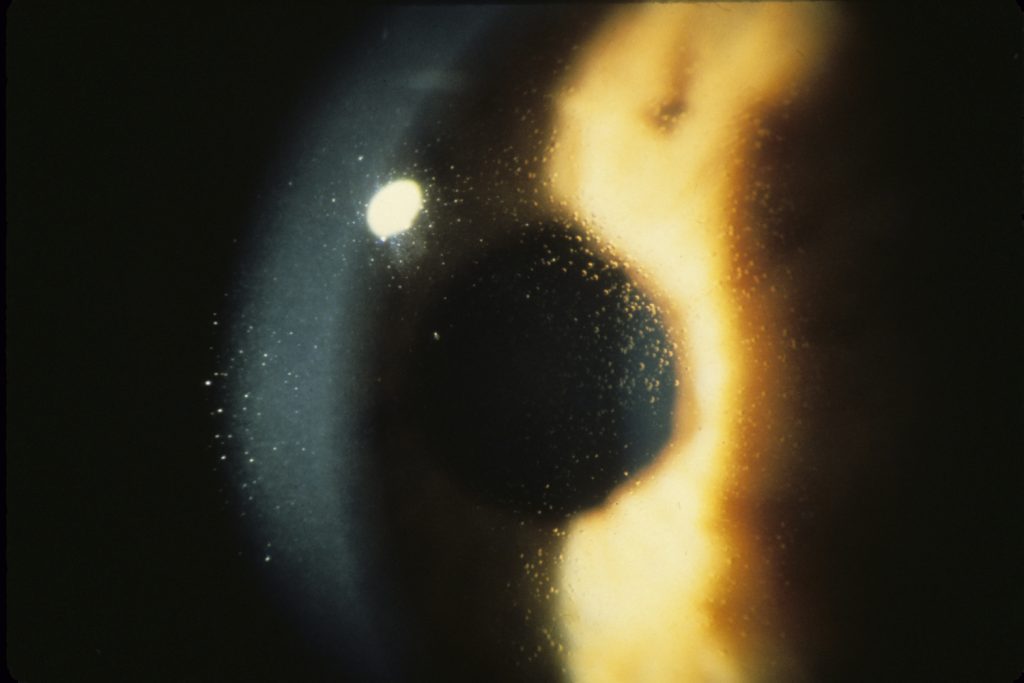
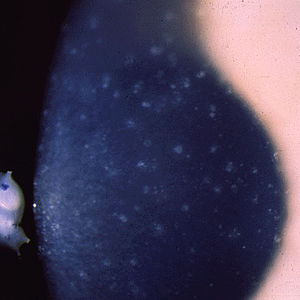
On slitlamp biomicroscopy, diffuse intra-epithelial microcystic changes were present within the entire corneal epithelium. Intraocular pressure (IOP) was normal and funduscopic examination disclosed pathologic myopic changes in both eyes.
A diagnosis was Meesmann Corneal Dystrophy (MCD) associated with amblyopia due to high myopia.
Meesmann Corneal Dystrophy (MECD) DISEASE entity
Meesmann Corneal Dystrophy (MECD) is a rare hereditary type of superficial corneal dystrophy that follows an autosomal dominant pattern of inheritance. It is characterized by the bilaterally symmetric development of intraepithelial microcysts that cause fragility of the anterior corneal epithelium.
Unlike most other corneal dystrophies, pathology in MECD manifests early in life and epithelial cysts may present already in the first years of life. The onset of symptoms during infancy or early childhood does not become noticeable or problematic until adulthood.
As the disorder slowly progresses, the number of tiny epithelial vesicles usually increases with age involving the central visual axis and mid-periphery of the cornea and can extend out to the limbus. The bubble-like blebs tend to be denser in the interpalpebral area and can be best visualized with retro illumination.
Most patients remain asymptomatic or may experience minor symptoms and minimal vision disturbances for years, while some suffer from recurrent episodes of corneal erosions resulting in lacrimation, photophobia, and deterioration in visual acuity, accompanied by irregular astigmatism and subepithelial scarring in some severe cases, particularly in elderly patients. Vision is seldom affected to a significant degree.
MANAGEMENT of Meesmann Corneal Dystrophy (MECD)
General treatment:
Meesmann Corneal Dystrophy (MECD) is a genetic disorder that persists throughout life. MECD usually remains an entirely asymptomatic condition that requires no treatment. For patients who experience minor intermittent symptoms of ocular irritation, a conservative therapeutic approach largely aimed at symptoms is preferred.
In rare cases of severe symptomatology or recurrent episodes of corneal erosions, surgical interventions may be required to prolong the reoccurrence of the disorder, and also lessen its severity.
Medical therapy:
Mild to moderate symptoms and Meesmann Corneal Dystrophy (MECD) -associated chronic eye dryness can be treated by using lubricating eye drops during the daytime and gel/ointment at night, but the majority of patients do not usually require further treatment.
Some physicians advocate the use of topical steroids to increase the stability of the epithelial basement membrane, while others prefer hypertonic saline, especially in gel or ointment form at night, which causes dehydration of the epithelium and promotes its attachment to the underlying layers.
Patching, either conventional or using a bandage soft contact lens, can be beneficial as it minimizes the mechanical effect of lid movement on the irregular corneal epithelium.
Surgery
A more severe phenotype of Meesmann Corneal Dystrophy (MECD), described by recurrent corneal erosions and secondary scarring, can complicate the clinical presentation of MECD and conservative therapy often proves to be unsuccessful.
Surgical treatment options aim at the removal of the pathological corneal epithelium and include superficial corneal debridement, superficial keratectomy with or without mitomycin C, phototherapeutic keratectomy (PTK), lamellar keratoplasty, and penetrating keratoplasty.
Although dystrophy frequently recurs after any of these treatments, in some cases, recurrence may be less severe, delayed, or not occur.
Superficial Mechanical Debridement of the epithelium can be useful in the management of RCE but is usually followed by the reappearance of symptoms.
Superficial Keratectomy is a safe technique for managing corneal erosions and although it may be curative, it is rarely warranted.
Phototherapeutic Keratectomy using a 193- nm excimer laser is the method of choice nowadays, replacing manual lamellar keratoplasty as the former treatment of choice. PTK can be repeated several times for the treatment of recurrent corneal erosions, thus postponing corneal transplantation (lamellar or even penetrating) for a long time.
This treatment achieves the removal of superficial corneal opacities, smoothing of the corneal surface, as well as correcting irregular astigmatism, and finally promoting the adherence of the epithelium to the underlying layers.
Lamellar and Penetrating Keratoplasty are seldom indicated for the treatment of MECD.
Rarely, a more severe phenotype with corneal erosions and significant scarring accompanied by a marked decrease in visual acuity may require treatment by keratoplasty or corneal grafting.
Although epithelium damage is likely to recur in grafts, the recurrent disease is often less severe. It is important to postpone grafting as long as possible because most patients require regrafting due to recurrences.
Surgical follow-up
Surgical procedures that aim to remove the abnormal corneal epithelium are not curative, as the dystrophy recurs in the regenerated epithelium, and therefore provide only temporary symptomatic relief. All surgical treatment options have a high risk of recurrence.
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
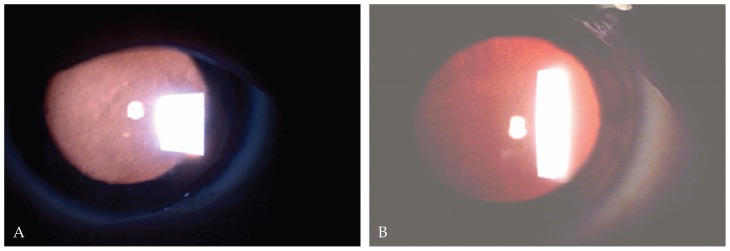
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Contributor: Christopher Kirkpatrick. Eye Rounds Org. The University of Iowa.
- Klintworth Orphanet Journal of Rare Diseases 2009 4:7 doi:10.1186/1750-1172-4-7
- Goldberg A, Schlötzer-Schrehardt U, Seiler T. Unilateral Meesmann’s dystrophy. Int Ophthalmol. 1997;21(3):117‐120. doi:10.1023/a:1026456232212.
- Schmidt-Erfurth U, Kohnen T. Juvenile Epithelial Dystrophy (Meesmann Dystrophy. In: Encyclopedia of Ophthalmology. Berlin: Springer; 2018:977-988.
- Prajna NV, Peyman GA, Hamada S, Maqsood S. Ch 69: Corneal Disorders in Children. In: Peyman’s Principles & Practice of Ophthalmology. Vol 1. 2nd ed. New Delhi: Jaypee Brothers; 2019:1183.
- Meesmann. Klinische und anatomische Untersuchungen über eine bisher unbekannte, dominant vererbte Dystrophia epithelialis corneae. Bericht der Deutschen ophthalmologischen Gesellschaft, Heidelberg, 1938, 52: 154-158.
- A. Meesmann, F. Wilke. Klinische und anatomische Untersuchungen über eine bisher unbekannte, dominant vererbte Epithel Dystrophie der Horn haut. Klinische Monatsblätter für Augenheilkunde, Stuttgart, 1939, 103: 361-391.
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE

