CASE REPORT
a 65-year-old man developed an abnormal vision in his left eye and presented to a hospital a few weeks after the initial presentation. Prior to this development, he had been physically well and had not had any history of ocular disease or previous injury.
On initial examination, the best-corrected visual acuity was 0.8 in the right and 0.3 in the left eye. Intraocular pressure was 15 mmHg in the right and 10 mmHg in the left eye. Light reflex was rapid in both eyes and the relative afferent pupillary defect was negative. Slit-lamp examination showed cataracts in both eyes.
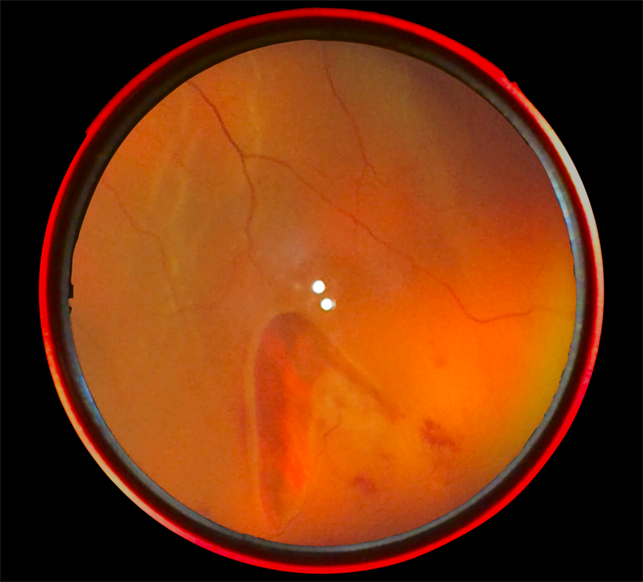
Fundoscopy revealed a horseshoe-like tear on the temporal side of the macula in the left eye. The tear size was 0.75 disc diameter. There was adhesion between the retinal tear and the vitreous. Fluorescein angiography revealed a nonperfusion area and the absence of any findings of retinal vein occlusion.
Horseshoe tears DISEASE entity
Horseshoe tears, also referred to as flap or U-shaped tears, are full-thickness breaks in the neurosensory retina that occur secondary to vitreoretinal traction. The apex of the flap is pulled anteriorly into the vitreous cavity while the base remains attached to the retina.
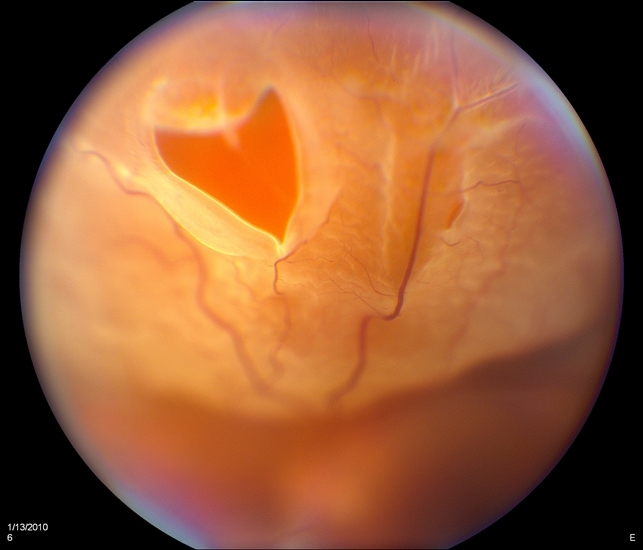
The most common cause of a horseshoe tear is a posterior vitreous detachment (PVD). Horseshoe tears are more common in the superotemporal quadrant followed by the superonasal quadrant.
Horseshoe tears frequently occur in middle-aged individuals and no statistical difference exists between men and women in the incidence of retinal breaks.
Horseshoe tears Risk Factors
Risk factors are:
Age: Increased incidence of retinal tears in adults is noted with increasing age.
Myopia: The prevalence of retinal breaks in myopic eyes is similar to that of eyes in the general population (11%). However, myopes account for 42% of all phakic RD and, therefore, myopia is considered a risk factor for retinal breaks that lead to RD.
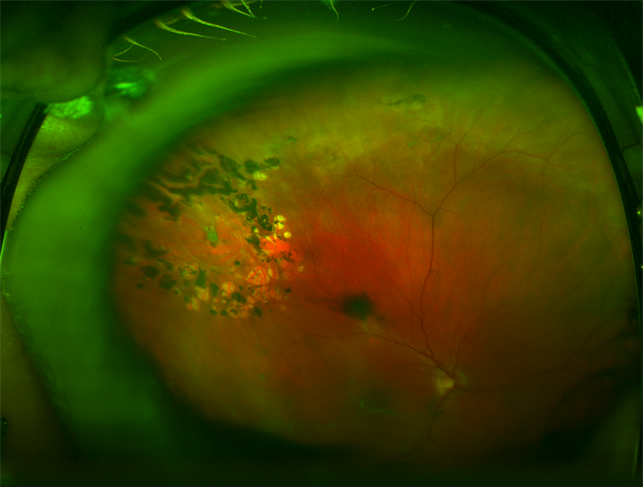
Lattice Degeneration: this is a condition in which peripheral retinal thinning is associated with liquefaction and separation of the overlying vitreous. It is often related to round retinal holes, but it can also be associated with flap tears at the edge of the lattice.
There is pronounced vitreoretinal adhesion at the margin of lattice lesions, which can predispose to retinal tears after PVD. These tears typically occur at the posterior margin or posterior lateral margin of lattice degeneration. This condition occurs in 5% of eyes and is more prevalent in moderate myopia.
Lattice degeneration is found in 30% of all eyes with rhegmatogenous retinal detachments. Long-term observational studies suggest that not all cases of flap tears develop clinically significant retinal detachment.
Penetrating trauma: can increase the risk of a retinal break either immediately after impact, due to direct retinal trauma, or later on due to vitreous traction on the peripheral retina.
Blunt trauma: is more commonly associated with retinal dialysis mainly located in the super-temporal periphery, but it can also cause other types of retinal breaks, such as horseshoe tears or macular holes.
Family history of retinal tears or retinal detachment
Previous ocular surgery
MANAGEMENT of Horseshoe tears
General treatment
The decision to treat a retinal tear is based on several factors, including symptomatology, patient age and systemic health, refractive error, location, age, type, size of the break; status of the fellow eye, lens status, and family history of retinal break and/or retinal detachment.
Medical therapy
Although some ophthalmologists consider that asymptomatic horseshoe tears may not be treated, others stress that all tears require treatment by retinopexy, either laser photocoagulation or cryotherapy. Any retinopexy performed must cover both the posterior aspect of the tear and its anterior corners.
This should be performed immediately after the diagnosis, and subsequent reviews are merely to determine that the retinopexy is adequately encompassing the defect.
Surgery
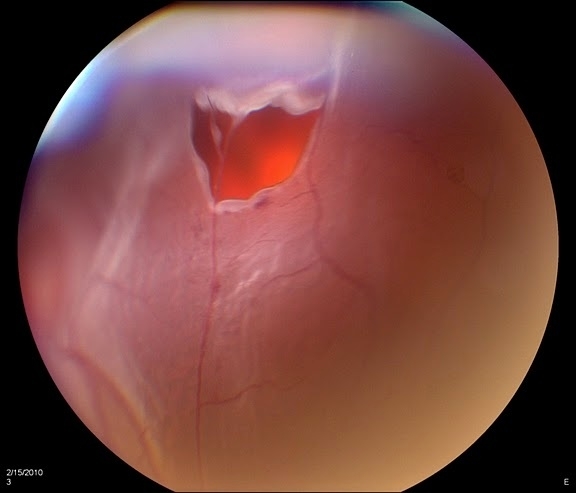
Any subretinal fluid around the tear indicates that a retinal detachment (most commonly rhegmatogenous) is present, and a surgical retinal detachment procedure is usually required for clinical retinal detachments, such as pars plana vitrectomy or scleral buckle.
If the subretinal fluid is minimal, cryotherapy can sometimes be successful on its own, however, this should be done rarely and only if appropriate and the eye should be closely monitored. Most subclinical detachments can be managed by laser or cryopexy.
Subclinical retinal detachment has been defined as the subretinal fluid of at least 1 disc diameter from the posterior edge of the break but not extending more than 2-disc diameters beyond the equator which does not affect the visual field.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
1. Byer NE., Long-term natural history of lattice degeneration of the retina. Ophthalmology 1989;96:1396–401.
2. Kun E., Gross and microscopic pathology in autopsy eyes. Part III. Retinal breaks without detachment. Am J Ophthalmol 1961; 51:369-391.
3. Haiman M.H., Burton T.C., Brown C.K., Epidemiology of retinal detachment. Arch Ophthalmol 1982; 100:289-292.
4. Byer N.E., What happens to untreated asymptomatic retinal breaks, and are they affected by posterior vitreous detachment? Ophthalmology 1998; 105:1045-1050
5. Davis M.D.: Natural history of retinal breaks without detachment. Arch Ophthalmol 1974; 92:183-194.
6. Smiddy W.E., Flynn H.W., Nicholson D.H., et al, Results and complications in treated retinal breaks. Am J Ophthalmol 1991; 112:623-631.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

