CASE REPORT
A 33-year-old male presented complaining of loss of vision in the lower half of the right eye for three weeks’ duration. When he became symptomatic he had been staying at the Siachen glacier (5472 meters above mean sea level) for three months.
Ten days after the onset of symptoms he came down to the plains and presented. He had no associated systemic disease and was a non-smoker. Ocular examination showed the best corrected visual acuity of 6/6 in both eyes.
There was a relative afferent pupillary defect in the right eye. The anterior segment of both eyes was normal with intraocular pressure (IOP) of 14mm Hg in both eyes.
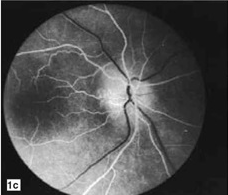
A Fundoscopy of the right eye showed pale disc edema in the superior half of the optic disc, while the left eye was normal. Fundus fluorescein angiography of the right eye showed initial hypofluorescence with late optic disc staining in the superior half.
Visual field examination (30-2 threshold list) on Humphrey’s perimeter showed an inferior altitudinal defect in the right eye with the normal visual field in the left eye. A diagnosis of High Altitude Retinopathy was confirmed.
DISEASE
High altitude retinopathy (HAR) encompasses a spectrum of pathological retinal changes occurring in unacclimatized individuals exposed to hypobaric hypoxia encountered at high altitudes.
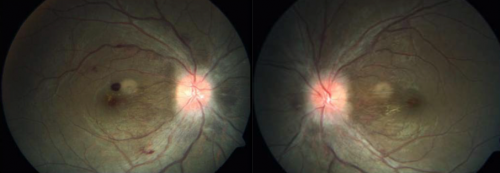
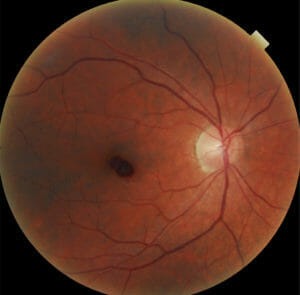
Affected individuals are usually asymptomatic and typical features, including retinal hemorrhages and papilledema, generally resolve spontaneously without adverse visual outcomes on the descent to lower altitudes.
High altitude retinopathy (HAR) is one of four clinical entities of high-altitude illness (HAI) that includes acute mountain sickness (AMS), high altitude cerebral edema (HACE), and high altitude pulmonary edema (HAPE).
HAR occurs with travel to elevations above 2500 meters (~8200 feet) and is generally characterized by symptoms of headache, nausea, vomiting, and tiredness, but may affect the lungs, brain, and eyes differently among individuals.

MANAGEMENT
General treatment:
High altitude retinopathy (HAR) is usually asymptomatic, and typical retinal changes are often only detected incidentally after descent to lower altitudes or not detected at all.
If vision-involving HAR develops at high altitudes, general treatment measures include immediate descent to lower altitudes and administration of supplemental oxygen.
Medical therapy:
The majority of cases of High altitude retinopathy (HAR) resolve spontaneously with no long-term adverse visual outcomes. Besides the general measures mentioned above, no specific therapies for HAR have been proven, although it may be necessary to treat the acute manifestations of altitude illness or the chronic ocular complications of the condition (e.g. retinal vein occlusion).
Medications such as NSAIDs, corticosteroids, and acetazolamide have been shown to have no impact on retinal hemorrhages The use of furosemide is inconclusive.
Although no systemic medications are indicated specifically for High altitude retinopathy (HAR), many are suggested for the other three clinical entities of high altitude illness (HAI): acute mountain sickness (AMS), high altitude cerebral edema (HACE), and high altitude pulmonary edema (HAPE):
- Carbonic anhydrase inhibitors: acetazolamide and methazolamide
- Steroids: budesonide, prednisone, and dexamethasone
- Bronchodilator drugs: salmeterol, theophyline and montelukast
- Selective inhibitors of phosphodiesterase type 5 (PDE5): tadalafil and sildenafil
- Calcium modulators: nifedipine and flunarizine
- Non-steroidal anti-inflammatory drugs (NSAIDs) and other analgesics: aspirin, carbasalate and ibuprofen.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Nieto Estrada VH, Molano Franco D, Medina RD, Gonzalez Garay AG, Martí-Carvajal AJ, Arevalo-Rodriguez I. Interventions for preventing high altitude illness: Part 1. Commonly-used classes of drugs. Cochrane Database Syst Rev. 2017 Jun 27;6(6): CD009761. doi 10.1002/14651858.CD009761.pub2. PMID: 28653390; PMCID: PMC6481751.
- Rennie D, Morrissey J. Retinal Changes in Himalayan Climbers. Arch Ophthalmol. 1975;93:395-400. doi:10.1001/archopht.1975.01010020409001.
- Shults WT, Swan KC. High Altitude Retinopathy in Mountain Climbers. Arch Ophthalmol. 1975;93:404-408. doi:10.1001/archopht.1975.010100204180.
- Schneider M, Bernasch D, Weymann J, Holle R, Bartsch P. Acute mountain sickness: influence of susceptibility, preexposure, and ascent rate. Med Sci Sports Exerc. 2002;34(12):1886–1891. doi:10.1097/00005768-200212000-00005.
- Bloch KE, Turk AJ, Maggiorini M, Hess T, Merz T, Barthelmes D, et al. Effect of ascent protocol on acute mountain sickness and success at Muztagh Ata, 7546 m. High Alt Med Biol. 2009;10(1):25–32. doi:10.1089/ham.2008.1043.
- McFadden DM, Houston CS, Sutton JR, Powles ACP, Gray GW, Roberts RS. High-Altitude Retinopathy. JAMA. 1981;245:581-586. doi:10.1001/jama.1981.03310310023016.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

