DISEASE
Ocular candidiasis is a well-known complication of candidemia. Candidemia has become increasingly prevalent in the hospital setting as a complication of surgery and with increased use of parenteral nutrition, central venous catheters, and treatment with broad-spectrum antibiotics.

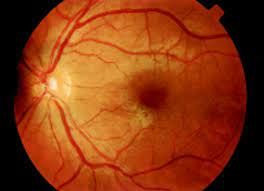
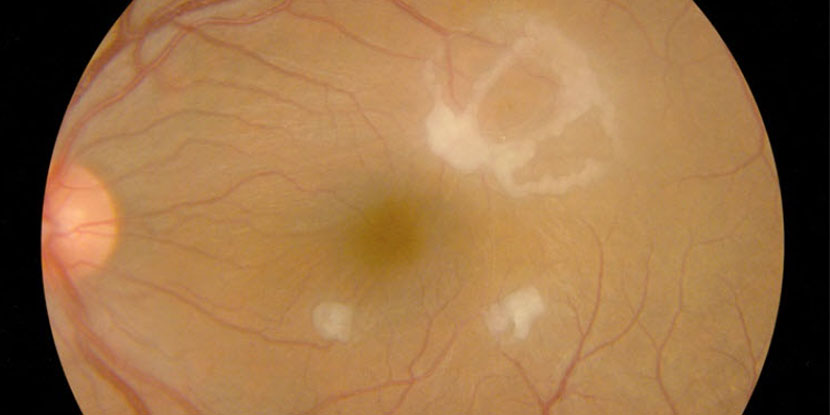
Systemic candidemia can lead to ocular candidiasis via hematogenous seeding of retinal and choroidal blood vessels and can have various ocular manifestations.
Ocular candidiasis can occur from exogenous or endogenous routes. Exogenous methods include trauma or direct inoculation from surgery or other procedures. Exogenous ocular candidiasis is uncommon in North America and Europe, and more commonly seen in tropical regions such as India.
Endogenous ocular candidiasis occurs from hematogenous seeding in the eye from transient fungemia, and while still rare, occurs most commonly in patients who are severely immunocompromised or who have indwelling catheters.
Diagnostic procedures
In cases where the clinical diagnosis is unclear, a vitreous tap to obtain intraocular fluid can be performed for gram staining and cultures. Intraocular culture specimens can also be obtained during pars plana vitrectomy.

While this is an effective method for obtaining intraocular culture specimens, this is often only performed in cases of severe endophthalmitis in conjunction with antifungal intravitreal injections for treatment.
When a patient has characteristic ocular candidiasis findings and known systemic candidiasis, ocular culture is not needed and this can be defined as probable ocular candidiasis. Positive growth of Candida species in conjunction with characteristic fundus features as described above is defined as proven ocular candidiasis.
B-scan ultrasound should be performed in cases where the retina is obscured by media opacity. In early cases, a fluorescein angiogram may demonstrate chorioretinitis.
MANAGEMENT
If possible, removal of the inciting cause of systemic candidemia is advised (e.g. removal or replacement of indwelling lines/catheters). Systemic antifungal therapy is targeted based on culture susceptibilities, and options include intravenous amphotericin B, azoles (e.g. voriconazole, fluconazole), and echinocandins (e.g. micafungin, caspofungin).
In general, initial therapy with an intravenous echinocandin is recommended for both non-neutropenic and neutropenic patients with candidemia. Fluconazole may be used as an alternative in non-neutropenic patients who are not critically ill.
However, as neutropenic patients are often placed on fluconazole prophylaxis, there has been an increasing number of Candida species with reduced susceptibility. In patients who are clinically stable, have repeat negative blood cultures, and have Candida species susceptible to fluconazole, step-down therapy to oral fluconazole may be pursued after 5-7 days.
Access to various medications will be dictated by region and the involvement of infectious disease specialists is recommended. A review of contemporary studies suggests that ocular candidiasis responds well to systemic medical management.
In the review by Breazzano et al., chorioretinitis was identified in 78 patients with resolution on systemic monotherapy.
Of the 19 endophthalmitis cases included in the review, 12 patients were treated with systemic therapy alone, 6 received combined systemic and local therapy (2 pars plana vitrectomy, 2 combined pars plana vitrectomy/tap and injection, and 2 taps and injection), and 1 patient improved solely with IV catheter removal.
Six of the 12 patients with endophthalmitis treated with systemic monotherapy died. Of the 6 surviving endophthalmitis patients treated with systemic monotherapy, complete ocular resolution occurred.
The patients who received both local intervention and systemic treatment achieved resolution with 3 patients having permanent vision loss. These results may be influenced by the severity of the disease.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Fraser VJ, Jones M, Dunkel J, Storfer S, Medoff G, Claiborne Dunagan W. Candidemia in a tertiary care hospital: Epidemiology, risk factors, and predictors of mortality. Clin Infect Dis. 1992;15(3):414-421. doi:10.1093/clind/15.3.414.
- Shah CP, McKey J, Spirn MJ, Maguire J. Ocular candidiasis: A review. Br J Ophthalmol. 2008;92(4):466-468. doi:10.1136/bjo.2007.133405.
- Son HJ, Kim MJ, Lee S, et al. Risk factors and outcomes of patients with ocular involvement of candidemia. PLoS One. 2019;14(9):1-13. doi:10.1371/journal.pone.0222356.
- Donahue SP, Greven CM, Zuravleff JJ, et al. Intraocular Candidiasis in Patients with Candidemia: Clinical Implications Derived from a Prospective Multicenter Study. Ophthalmology. 1994;101(7):1302-1309. doi:10.1016/S0161-6420(94)31175-4.
- Khalid A, Clough LA, Symons RCA, Mahnken JD, Dong L, Eid AJ. Incidence and clinical predictors of ocular candidiasis in patients with Candida fungemia. Interdiscip Perspect Infect Dis. 2014;2014. doi:10.1155/2014/650235.
- Abusamra K. Candidiasis. In: Foster CS, Anesi SD, Chang PY, eds. Uveitis: A Quick Guide to Essential Diagnosis. Springer International Publishing; 2021:189-191. doi:10.1007/978-3-030-52974-1_41.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

