CASE REPORT
A 51-year-old healthy female underwent uneventful cataract surgery in her right eye. During the procedure, viscoelastic and vancomycin (1.0 mg/0.2 mL) were injected into the anterior chamber.
Visual acuity on the first postoperative day was 20/20 and no other postoperative complication was detected. On the seventh postoperative day, the patient complained of acute painful visual deterioration. Visual acuity was 20/32 in her right eye with the minimal anterior chamber and vitreous reaction, not suggestive of endophthalmitis.
She was referred to a clinic 2 days later (post-op 9 days) for further investigation. Ophthalmic examination revealed best corrected visual acuity of 20/32 and 20/25 in the right and left eye respectively. Intraocular pressure was 15 mmHg in both eyes, and pupil reaction was normal.
A slit lamp examination of the right eye revealed 1+ cell in the anterior chamber and 1+ cell in the anterior vitreous.
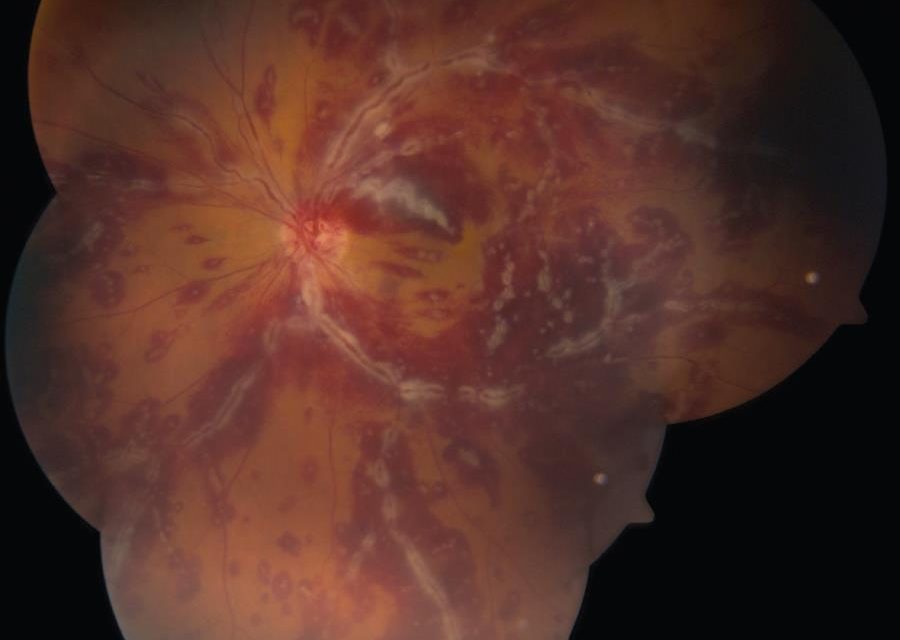
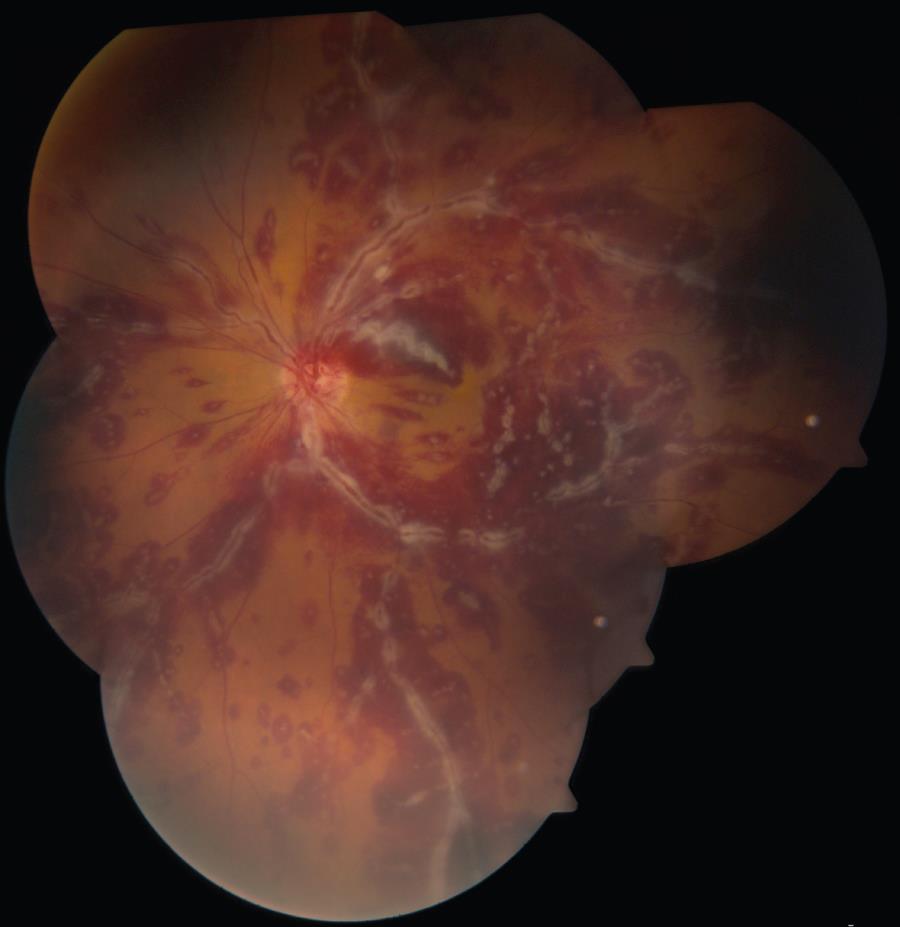
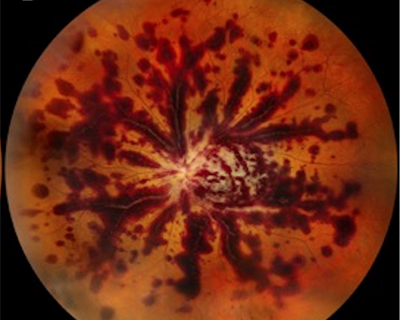
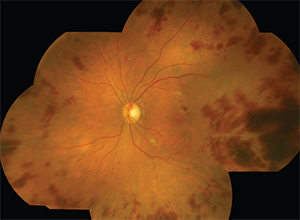
Fundus examination of the right eye was notable for mild vitritis, vascular attenuation, and peripheral artery occlusion, as well as scattered intraretinal and perivascular hemorrhages.
Fluorescein angiography revealed delayed retinal filling, peripheral vascular occlusion, extended areas of non-perfusion, and scattered areas of perivascular staining. The optical coherence tomography examination was unremarkable.
A 6 × 6 zone was acquired using optical coherence tomography angiography demonstrating the junction between perfusion and non-perfusion areas showing the choroidal vasculature intact.
Diagnosis of hemorrhagic occlusive retinal vasculitis (HORV) was made.
DISEASE
Hemorrhagic occlusive retinal vasculitis (HORV) has been described as a very rare but potentially devastating complication occurring after cataract surgery in which intraocular vancomycin is used.
It has a delayed onset and is associated with retinal hemorrhages, vascular nonperfusion, and venous sheathing. The severity appears to be worse when the second eye has undergone cataract surgery in which vancomycin is used.
Visual acuity is typically severely decreased. In the original descriptions by Nicholson et al and Witkin et al, presenting visual acuities were very poor. Patients typically presented 1 to 14 days after successful cataract surgery.
However, patients may present from 1-21 days postoperatively (mean 8 days). Visual acuity outcomes were poor: 4 of 11 eyes were NLP and the others were less than 20/100. A larger series of 23 patients and 36 eyes noted the following characteristic features of HORV:
- Typically postoperative day 1 undilated examination is unremarkable
- Delayed onset vision loss
- Mild anterior chamber and vitreous inflammation
- Sectoral retinal hemorrhages in areas of ischemia
- A predilection for venules and peripheral involvement
Diagnostic procedures
- Fundus photo shows vasculitis, hemorrhage, and retinal whitening in some cases.
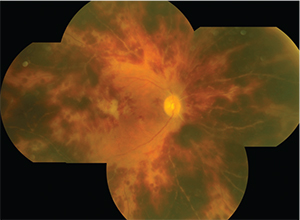
- Fundus fluorescein angiogram shows severe capillary nonperfusion.
- Optical coherence tomography may show inner retinal hyperreflectivity, increased thickness of the inner retina, and cystoid macular edema (rare).
- B-scan ultrasonography is needed in cases of media haze due to vitreous hemorrhage.
MANAGEMENT
- Systemic and topical corticosteroids may help. Early anti-VEGF intravitreous injection and PRP may prevent neovascular glaucoma
- Avoid vancomycin for suspected endophthalmitis
- Avoid vancomycin use in the second eye
The recommendations for Hemorrhagic Occlusive Retinal Vasculitis (HORV) are as follows:
Considerations for intraocular vancomycin use
- Because Hemorrhagic Occlusive Retinal Vasculitis (HORV) seems extremely rare, each surgeon should weigh the potential risk of HORV associated with vancomycin against the risk of endophthalmitis.
- Reconsider using vancomycin with close sequential bilateral cataract surgery, especially if immediate sequential same-day bilateral surgery is performed.
- Surgeons using intraocular vancomycin with sequential cataract surgery should be aware that in addition to delayed onset, HORV may not cause symptoms in the first eye, and a dilated retinal examination may be the only way to detect it.
- Surgeons desiring an alternative to vancomycin for intracameral prophylaxis may consider cefuroxime or moxifloxacin.
Recommendations for the management of HORV
- Avoid intravitreal vancomycin if HORV is suspected.
- Consider an ocular or systemic workup, or both, for other syndromes (e.g., viral retinitis) if the diagnosis is unclear.
- Aggressive systemic and topical corticosteroids; consider periocular or intraocular steroids.
- Early anti-VEGF treatment.
- Early pan-retinal photocoagulation.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Nicholson LB, Kim BT, Jardon J, et al. Severe bilateral ischemic retinal vasculitis following cataract surgery. Ophthalmic Surg Lasers Imaging Retina. 2014;45(4):338-342.
- Witkin AJ, Shah AR, Engstrom RE, et al. Postoperative hemorrhagic occlusive retinal vasculitis: expanding the clinical spectrum and possible association with vancomycin. Ophthalmology. 2015;122(7):1438-1451.
- Witkin AJ, Chang DF, Jumper JM, et al. Vancomycin-Associated Hemorrhagic Occlusive Retinal Vasculitis: Clinical Characteristics of 36 Eyes. Ophthalmology. 2017;124(5):583–595. doi:10.1016/j.ophtha.2016.11.042
- Todorich B. et al. Vancomycin-Associated Hemorrhagic Occlusive Retinal Vasculitis: A Clinical-Pathophysiological Analysis. Am J Ophthalmol 2018;188:131–140.
- Andre J. Witkin, MD, David F. Chang, MD, J. Michael Jumper, MD, Steve Charles, MD, FACS, Dean Eliott, MD, Richard S. Hoffman, MD, Nick Mamalis, MD, Kevin M. Miller, MD, Charles C. Wykoff, MD, PhD. Vancomycin-Associated Hemorrhagic Occlusive Retinal Vasculitis Ophthalmology 2017;124:583-595
- Arepalli S, Modi YS, Deasy R, Srivastava SK. Mild Bilateral Hemorrhagic Occlusive Retinal Vasculitis Following Intracameral Vancomycin Administration in Cataract Surgery. Ophthalmic Surg Lasers Imaging Retina. 2018 May1;49(5):369-373.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE