CASE REPORT
A 40-year-old female presented with complaints of sudden, painless visual disturbances in the left eye. A mastectomy was performed six years ago due to a breast carcinoma, which required radiation therapy.

Visual acuity was tested on the right eye by counting fingers from 1 meter away and on the left eye 0,9-1,0 by Snellen. Intraocular pressure was 18 mmHg in the right eye and 16 mm Hg in the left eye. A slit lamp biomicroscopy showed a normal appearance.
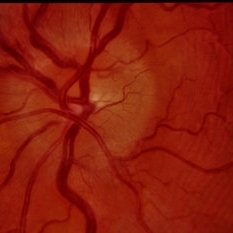
A posterior segment examination showed a swollen, enlarged, and blurred optic disc, with a dilated capillary net. The whole posterior segment was covered with a golden-yellow lesion on the right eye.
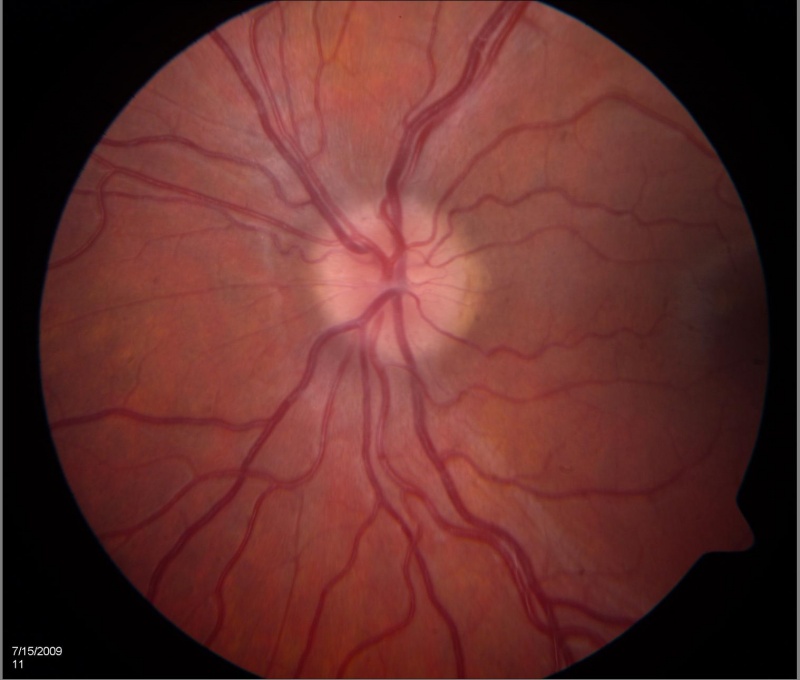
The optic disc in the left eye had a normal appearance but there were yellow, oval-shaped lesions (similar to that in the right eye) present in the posterior pole temporally area. FA showed dilated capillaries of the optic disc with leaking in the early phase and diffuse hyper fluorescence that continued during the late phase.
Large caliber intralesional vessels, relatively hyperfluorescent in the early phase of angiography, and diffuse hyperfluorescent in the late phase of angiography were presented together with the leaking from the whole posterior pole.
The ultrasonography B-scan (USG) showed a prominent optic nerve with a widened optic nerve sheath. The OCT demonstrated marked papilledema.
Papilledema disease entity
Papilledema is a term that is exclusively used when disc swelling is secondary to increased intracranial pressure (ICP). It must be distinguished from optic disc swelling from other causes which are simply termed “optic disc edema”.
Papilledema must also be distinguished from pseudo-papilledema such as optic disc drusen. Since the root cause of papilledema is increased intracranial pressure (ICP) this is an alarming sign which may presage such entities as brain tumors, CNS inflammation, cerebral venous thrombosis, or idiopathic intracranial hypertension (IIH).
As noted above, papilledema is due to increased intracranial pressure from any cause. Normal ICP is typically less than 250 mm of water in adults when measured with a manometer and is less than 280 mm of water in children.
Papilledema results from orthograde axoplasmic flow stasis at the optic nerve head leading to edema of the nerve from the increased intracranial pressure pressing on the nerve behind the eye. Continued pressure can result in loss of axons and eventual optic atrophy secondary to intraneuronal ischemia ultimately causing vision loss.
With optic atrophy, there is little or no edema seen even with continuing increased intracranial pressure since dead fibers don’t swell.
Increased intracranial pressure can be caused by five patho-mechanisms:
- When the skull is too small for the brain (e.g. craniosynostosis)
- When the brain volume becomes too large for the skull such as a space-occupying lesion (e.g. tumor, hemorrhage), or brain edema ( e.g. trauma)
- When there is obstruction of the cerebrospinal fluid (CSF) flow (e.g. colloid cyst obstructing the foramen of Monroe)
- Increased production of CSF (e.g. choroid plexus papilloma)
- Reduced absorption of CSF (e.g. meningitis, cerebral venous thrombosis)
The time course for the development of papilledema may be weeks if there is only a slow and mild rise in intracranial pressure, but severe and rapid changes in pressure can cause papilledema to present within a few hours to a day.
The mechanism of Idiopathic intracranial hypertension is not clearly understood however proposed mechanisms include increased venous sinus pressure from venous sinus stenosis, and reduced absorption to name a few.
Papilledema MANAGEMENT
Management goals are:
(1) Treating the underlying cause, (2) saving vision, and (3) symptomatic relief (e.g. headache):
- treating the underlying cause
- If malignant hypertension was found, then the patient must be sent to the emergency department for further management. Even with malignant hypertension cases, the patient with papilledema should still proceed with neuro-imaging
- If a mass is present, primary therapy should be directed toward that lesion (e.g., surgery)
- If acute cerebral venous thrombosis was seen, the patient must be sent to the thrombosis team immediately. It is best to avoid acetazolamide in cerebral venous thrombosis as it can precipitate the condition, however, it can later be added on when the patient has started on anti-coagulation
- Medications (tetracyclines, vitamin A analogs, etc.) are felt to be causative so they should be discontinued.
- saving vision & 3. symptomatic relief (e.g. headache)
- treat the underlying cause
- Medications to lower ICP
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Lee A, Rigi M, Al marzouqi S, Morgan M. Papilledema: epidemiology, etiology, and clinical management 2015;7-47.
- Keira A Markey, Susan P Mollan, Rigmor H Jensen, Alexandra J Sinclair. Understanding idiopathic intracranial hypertension: mechanisms, management, and future directions.Lancet Neurol. 2016 Jan;15(1):78-91. doi: 10.1016/S1474-4422(15)00298-7. Epub 2015 Dec 8. PMID: 26700907DOI: 10.1016/S1474-4422(15)00298-7.
- Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology. 2013 Sep 24;81(13):1159-65. doi: 10.1212/WNL.0b013e3182a55f17. Epub 2013 Aug 21. PMID: 23966248.
- Jacks A, Miller N. Spontaneous retinal venous pulsation: etiology and significance. J Neurol Neurosurg Psychiatry. 2003;74:7–9.
- Reference: Frisen L. Swelling of the optic nerve head: A staging scheme. J Neurol Neurosurg Psychiatry 1982; 45:13-18.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE


