CASE REPORT
DISEASE
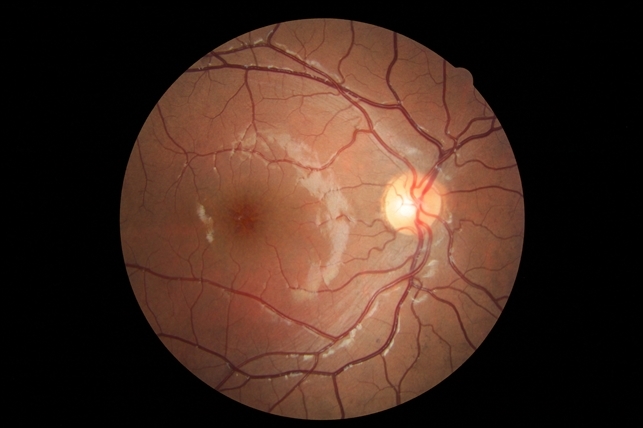
X-linked Retinoschisis or X-Linked Juvenile Retinoschisis is a rare congenital disease of the retina caused by mutations in the RS1 gene, which encodes retinoschisis, a protein involved in intercellular adhesion and likely retinal cellular organization.
X-linked retinoschisis has also been referred to as: juvenile retinoschisis, congenital retinoschisis, juvenile macular degeneration/dystrophy, degenerative retinoschisis, and vitreous veils of the retina.
X-linked retinoschisis, with a prevalence of about 1 in 15,000 to 30,000, is one of the main causes of juvenile macular degeneration in males. It is characterized by symmetric bilateral macular involvement beginning in the first decade of life.
It is caused by a large variety of mutations in the RS1 gene on Xp22.1-p22.3, which encodes the protein retinoschisis. This protein is involved in intercellular adhesion and likely retinal cellular organization. X-linked retinoschisis is inherited in an X-linked manner with complete penetrance and variable expressivity.
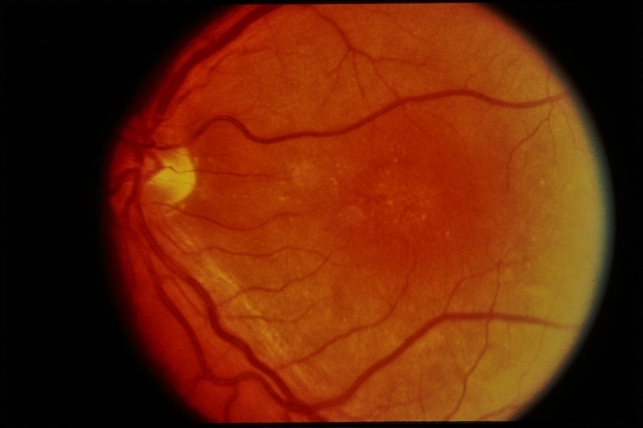
Most affected individuals are males, as heterozygous females are rarely affected. However, retinoschisis has been reported in non-consanguinous females. The phenotype can be markedly variable even within the same genotype and can involve the peripheral retina.
MANAGEMENT
For those below 10 years old: Annual evaluation by a pediatric ophthalmologist or retina specialist.
Patient education: Avoid head trauma and high-contact/impact sports due to the increased risk of retinal detachment.
Amblyopia: Treat amblyopia, especially in cases of severe retinoschisis, hypermetropia, or following surgery for vitreous hemorrhage or retinal detachment.
Genetic counseling: male patients should be counseled that they will pass the mutation to all daughters (who will most likely be asymptomatic heterozygote carriers), but will not pass the mutation to sons.
Female carriers have a 50% chance of passing the mutation – all sons who inherit the mutation will be affected, and daughters who inherit the mutation will most likely be asymptomatic carriers.
For those with low vision: Low vision aids (large-print textbooks), preferential seating in the front of the classroom, and handouts with high contrast.
Medical therapy
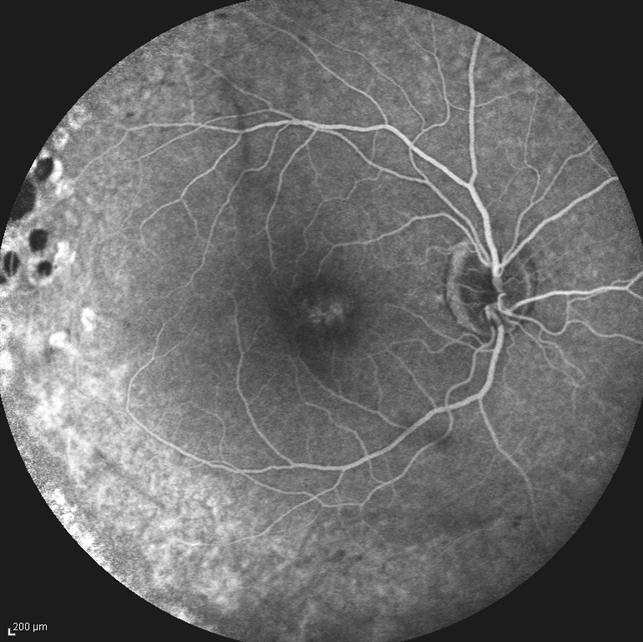
Carbonic anhydrase inhibitors may help to improve the schisis cavities seen on OCT. Topical dorzolamide or systemic acetazolamide have both been reported to be beneficial in improving the cystic-appearing spaces on OCT.
Clinical improvement can be monitored with visual acuity improvements and reduction in the cystic fluid on OCT. Gene therapy with intra-ocular RS1 in knockout mice has restored b-wave function. In 2015, two human XLRS gene therapy trials were initiated:
- The NEI trial is evaluating the safety of a gene transfer vector (AVV-RS1) in humans. It found closure of schisis cavities in one individual at higher dosing, which also caused ocular inflammation.
- The AGTC trial is evaluating the safety and efficacy of a recombinant adeno-associated virus vector expressing retinoschisis (rAAV2tYF-CB-hRS1) in patients with X-linked retinoschisis.
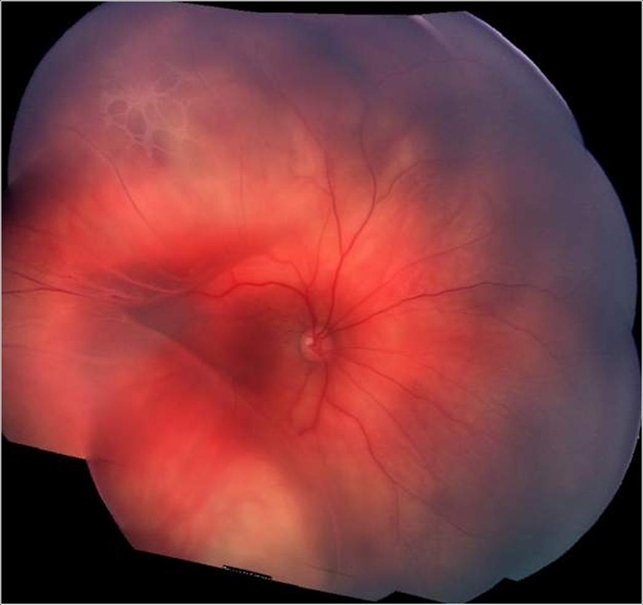
Surgery
- Complications such as retinal detachment and vitreous hemorrhage may require surgical intervention such as vitrectomy or scleral buckling.
- Laser photocoagulation may prevent retinal detachment. However, it may also induce detachment by creating iatrogenic retinal breaks. Thus, the prophylactic laser is controversial.
- External drainage has also been attempted.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- American Academy of Ophthalmology. X-linked juvenile retinoschisis.
- Sikkink SK, Biswas S, Parry NRA, Stanga PE, Trump D. X-linked retinoschisis: an update. Journal of Medical Genetics. 2007 Apr 1;44(4):225–32.
- Sieving PA, MacDonald IM, Hoang S. X-Linked Congenital Retinoschisis. 2003 Oct 24 [Updated 2020 Nov 5]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1222/
- Saleheen D, Ali A, Khanum S, Ozair MZ, Zaidi M, Sethi MJ, et al. Molecular analysis of the XLRS1 gene in 4 females affected with X-linked juvenile retinoschisis. Can J Ophthalmol. 2008 Oct;43(5):596–9.
- Rodríguez FJ, Rodríguez A, Mendoza-Londoño R, Tamayo ML. X-linked retinoschisis in three females from the same family: a phenotype-genotype correlation. Retina (Philadelphia, Pa). 2005 Jan;25(1):69–74.
- Grayson C, Reid SNM, Ellis JA, Rutherford A, Sowden JC, Yates JRW, et al. Retinoschisin, the X-linked retinoschisis protein, is a secreted photoreceptor protein and is expressed and released by Weri–Rb1 cells. Hum Mol Genet. 2000 Jul 22;9(12):1873–9.
- Yassur Y, Nissenkorn I, Ben-Sira I, Kaffe S, Goodman RM. Autosomal Dominant Inheritance of Retinoschisis. American Journal of Ophthalmology. 1982 Sep 1;94(3):338–43.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

