CASE REPORT
A 69-year-old female patient complained of progressive vision loss. Her parents were first cousins. The patient had been a smoker for 15 years. She had a past medical history of hyperlipidemia and hypothyroidism.

Upon a comprehensive ophthalmic evaluation, the patient was found to have the best corrected visual acuity of counting fingers at 5’ and 3’ in the right and left eyes, respectively.
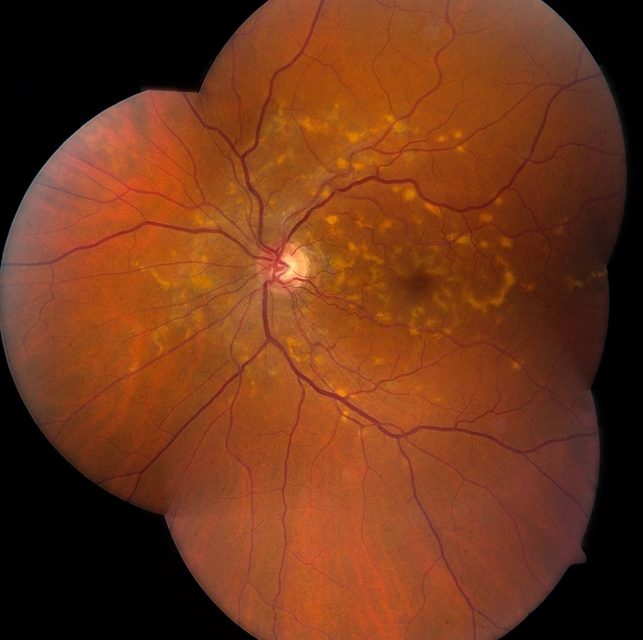
Retinoscopy showed a refraction of –1.00 + 0.50×70 and –2.00 + 1.00×5 in the right and left eyes, respectively. The patient had pale optic discs with extensive deep atrophy of the central macula, epithelial pigment hyperplasia, and other areas of multifocal atrophy in the right eye.
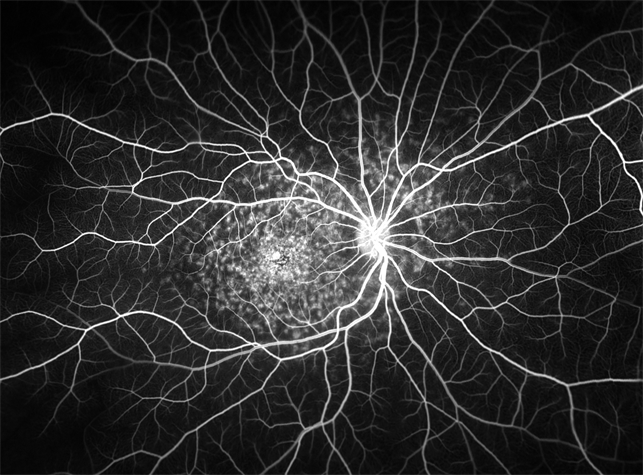
In addition, the patient had macular atrophy in the left eye. In the patient’s fundus autofluorescence (FAF) imaging, there was evidence of central hypo autofluorescence of the macula, with diffuse outward centrifugal extension from its center to its periphery.
Macular optical coherence tomography (OCT) determined that the average macular thickness was 191 µM and 193 µM in the right and left eyes, respectively. Macular volume was 6.9 mm3 and 7.0 mm3 in the right and left eyes, respectively. No macular edema, cysts, or subretinal fluid was found in either eye.
A visual field test revealed that the patient had mean deviations of –23.75 dB and –24.56 dB in the right and left eyes, respectively. Pattern standard deviations were +3.69 dB and +4.69 dB in the right and left eyes.
The results of a full-field electroretinogram (ERG) showed a normal rod response and decreased cone response, bilaterally. For these reasons, a clinical diagnosis of Stargardt disease was made.
DISEASE
Stargardt disease (STGD) is the most common childhood recessively inherited macular dystrophy. The condition has a genetic basis due to mutations in the ABCA4 gene, on chromosome 1, which encodes a retinal transported protein; it results from the accumulation of visual cycle kinetics-derived byproducts in the retinal pigmented epithelium (RPE) with secondary photoreceptor dysfunction and death.
The most common symptom of Stargardt disease is a slow loss of central vision in both eyes. Some people lose their central vision more quickly than others.
Other symptoms may include:
- Gray, black, or hazy spots in the center of your vision
- Sensitivity to light
- Needing more time for your eyes to adjust between light and dark places
- Color blindness
Some people with Stargardt disease may also lose their side (peripheral) vision.
MANAGEMENT
Stargardt disease remains an incurable condition. Current therapeutic options include photoprotection and low-vision aids. Pharmacological slow-down of the visual cycle, gene therapy, and other treatment options aim to prevent lipofuscin accumulation and represent prospects of long-term visual rescue.
Unbound all-trans-retinal induces photo-oxidative damage to the unusually sensitive ABCA4, further compromising its function. Given that Stargardt patients already have impaired ABCA4 function and increased levels of all-trans-retinal trapped inside their photoreceptors, it is logical to think that these patients would be extremely sensitive to light exposure.
Furthermore, it has been demonstrated that di-retinoid-pyridinium-ethanolamine (A2E) does not accumulate in the RPE of abca4 knockout mice kept in total darkness. Thus, Stargardt patients should be advised to avoid direct sunlight exposure. Ultraviolet-blocking sunglasses are a useful option.
Vitamin A supplementation has been regarded as a therapeutic option for certain retinal degenerative conditions such as retinitis pigmentosa.
However, recent data suggests that in ABCA4-mediated disease, vitamin A supplementation accelerates the accumulation of lipofuscin pigments in the RPE. Long-term vitamin supplementation increases the formation of vitamin A dimers which favor lipofuscin synthesis and deposition.
Therefore, Stargardt patients should avoid vitamin A supplementation. In contrast, long-term administration of deuterium-enriched vitamin A (i.e. C20-D3-vitamin-A), may have a beneficial effect since this compound prevented vitamin A dimerization in the murine model of Stargardt disease.
Isotretinoin has reportedly been capable of dampening A2E deposition in the RPE of abca4 knockout mice. Considerable side effects associated with chronic intake of isotretinoin prevent its chronic use in humans.
Stargardt disease is a preferred target for gene replacement therapy. Like in Leber Congenital Amaurosis (LCA), from which the most astonishing results of human ocular gene therapy have been obtained, the replacement of the mutant ABCA4 gene by its wild-type counterpart may produce positive results, as those observed in RPE65 gene trials.
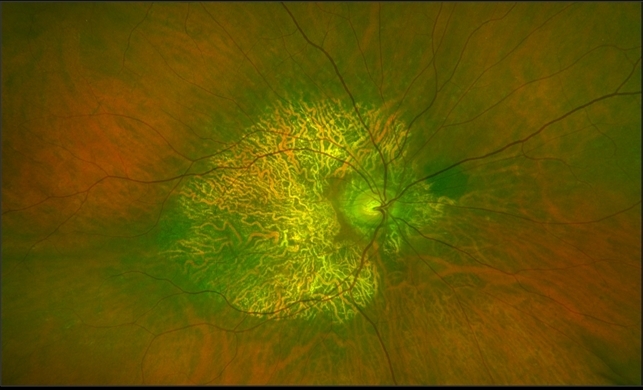
Given Stargardt is a retinal degeneration, the identification of viable photoreceptors plays a central role in the selection of patients amenable to gene therapy. Thus, retinal imaging is essential to assess photoreceptor viability, when selecting patients for gene therapy.
High-definition OCT and Adaptive Optics technology enhance lateral resolution in retinal images up to 3-4μm, allowing the visualization of individual photoreceptors.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Boyd K, Janigian RH. Juvenile Macular Degeneration. American Academy of Ophthalmology. EyeSmart® Eye health.
- Boyd K, Vemulakonda GA. Stargardt Disease. American Academy of Ophthalmology. EyeSmart® Eye health.
- Cremers FPM, Lee W, Collin RWJ, Allikmets R. Clinical spectrum, genetic complexity and therapeutic approaches for retinal disease caused by ABCA4 mutations. Prog Retin Eye Res. 2020 Nov;79:100861. doi: 10.1016/j.preteyeres.2020.100861. Epub 2020 Apr 9. PMID: 32278709; PMCID: PMC7544654.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE