CASE REPORT
A 48-year-old male with a history of hypertension and hypercholesterolemia presented with a two-week history of sudden, painless visual disturbances in his right eye, including floating spots and flashing lights in the nasal visual field.
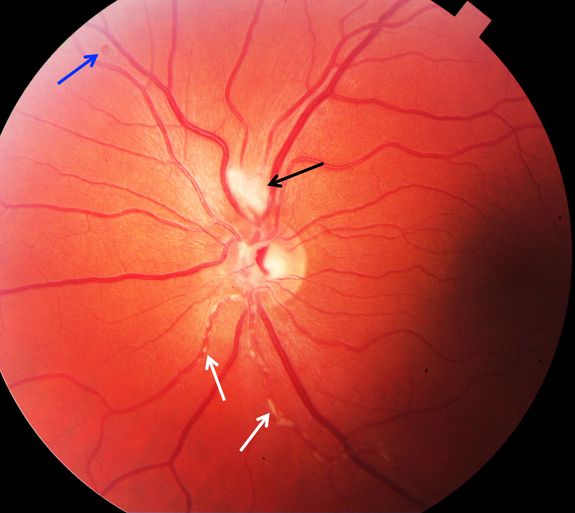
On examination, his right eye had a visual acuity of 20/30, while the left eye was 20/20. Fundus examination of the right eye revealed yellowish-white plaques along arterioles without macular involvement, alongside a relative afferent pupillary defect (RAPD).
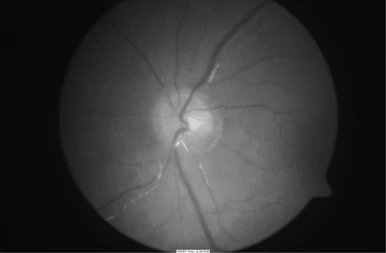
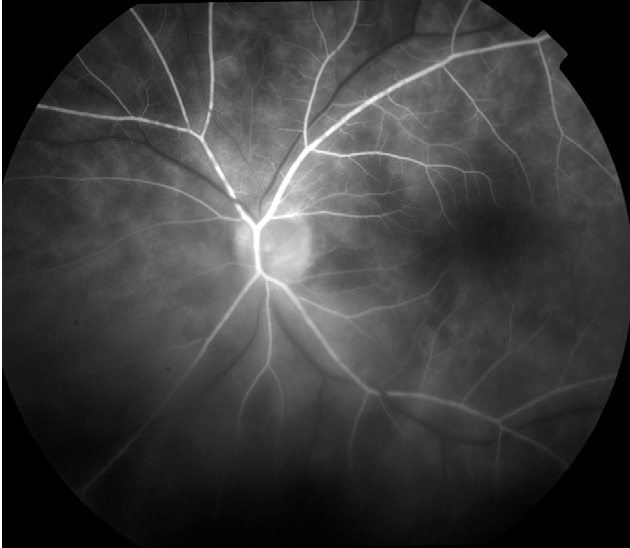
No intraocular inflammation or other abnormalities were noted. Diagnostic workup included optical coherence tomography (OCT), fluorescein angiography (FA) indicating arterial wall staining and dye leakage at plaque sites, and blood tests for autoimmune markers (ANA and antiphospholipid antibodies), all of which were negative. The diagnosis of Kyrieleis plaques was confirmed.
Kyrieleis Plaques entity
Kyrieleis plaques are also referred to as “Kyrieleis vasculitis”, “Kyrieleis arteriolitis”, “nodular periarteritis”, “segmental retinal periarteritis” or “segmental retinal arteritis” represent a rare fundus examination finding, first described in an eye with presumed tuberculous uveitis by Werner Kyrieleis, in 1933.
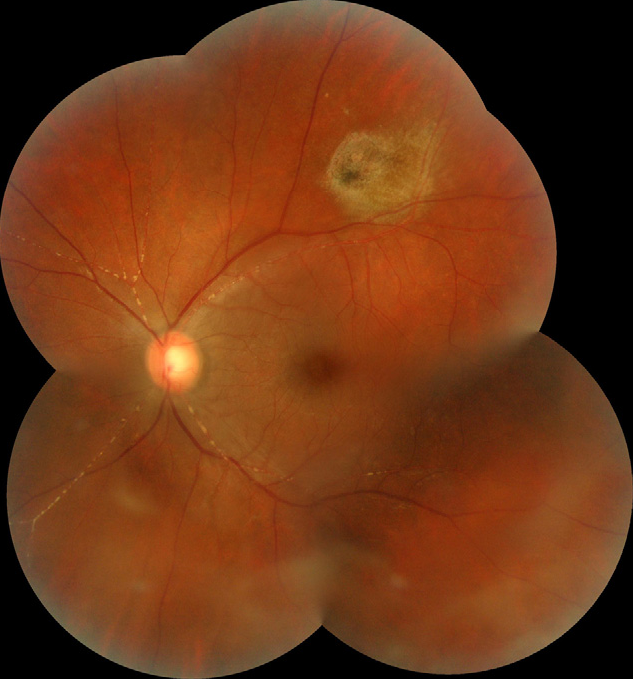
They appear as multiple, segmental yellowish-white lesions within the retinal arteries, in a beaded pattern reported both in infectious and non-infectious inflammatory posterior uveitis. These plaques are usually reversible.
The etiology of Kyrieleis plaques is unknown but they always reflect severe intra-ocular inflammation. They have been typically associated with infectious posterior uveitis, and Toxoplasma gondii is the most frequently reported cause.
Treponema pallidum, Mycobacterium tuberculosis, Varicella-Zoster Virus, Cytomegalovirus, Herpes Simplex Virus- 1 and 2, and Rickettsia conorii are other common agents.
Kyrieleis arteritis in association with Behçet disease has also been described. Kyrieleis plaques are also described as a clinical feature of Brolucizumab-Associated Retinal Vasculitis and Intraocular Inflammation.
The pathophysiology of these plaques is not completely known, and there is still a lot to discover about the composition of the whitish deposits and their exact location within the arteries.
Various hypotheses have been proposed, though. Griffin and Bodian, in 1959, speculated that the plaques represented exudates migration from an adjacent retinochoroiditis focus to the periarterial sheaths.
In 1971, Orzalesi and Ricciardi hypothesized that these deposits constituted cellular and inflammatory material within the arterial walls. Wise proposed that they were arteriosclerosis lesions.
Recently, a study based on multimodal retinal imaging, suggested that the plaques do not represent periarterial or endoluminal injury, but the involvement of the arterial endothelium.
Diagnosis of Kyrieleis Plaques
Like other forms of retinal vasculitis, the diagnosis of Kyrieleis is clinical, based on the fundoscopic examination, and supported by ancillary tests namely fluorescein angiography (FA), indocyanine green (ICG) angiography, fundus autofluorescence (FAF), and optical coherence tomography (OCT).
Fundoscopy
On the Smartphone Fundoscopy, Kyrieleis plaques appear as focal yellowish-white deposits, looking like atheromatous plaques, segmentally distributed along the retinal arteries.
As previously mentioned, these plaques always occur in association with intra-ocular inflammation, and typically, an active focus of chorioretinitis is present near the affected arteries.
Sometimes, the plaques can only be visible once the severe intraocular inflammation has resolved. Kyrieleis plaques involve exclusively the arterial and glisten and often look like calcific lesions.
Kyrieleis Plaques MANAGEMENT
The management of Kyrieleis arteritis depends on the underlying etiology. The control of intraocular inflammation is the primary goal.
Although associated with severe ocular inflammation, Kyrieleis plaques are a benign finding, that does not worsen the prognosis of the underlying uveitis.
Generally, with adequate treatment, there is a complete disappearance of the plaques (usually after the resolution of vitritis) without sequelae 5.
However, the plaques can persist long after the resolution of chorioretinitis and discontinuation of therapy.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Kyrieleis W. [Discontinuous reversible arteriopathy in uveitis]. Albrecht Von Graefes Arch Ophthalmol. 1950;150(5-6):600-13.
- Francés-Muñoz E, Gallego-Pinazo R, López-Lizcano R, García-Delpech S, Mullor JL, Díaz-Llopis M. Kyrieleis’ vasculitis in acute retinal necrosis. Clin Ophthalmol. 2010;4:837-8.
- Goel N, Sawhney A. Kyrieleis plaques associated with Herpes Simplex Virus type 1 acute retinal necrosis. Saudi J Ophthalmol. 2016;30(2):144-7.
- Pichi F, Veronese C, Lembo A, Invernizzi A, Mantovani A, Herbort CP, et al. New appraisals of Kyrieleis plaques: a multimodal imaging study. Br J Ophthalmol. 2017;101(3):316-21.
- Mahjoub A, Ben Abdesslem N, Zaafrane N, Sellem I, Sahraoui F, Nouri H, Hadj RB, Ben Alaya A, Krifa F, Hachemi M. Kyrieleis arteritis associated with toxoplasmic retinochoroiditis: A case report. Ann Med Surg (Lond). 2022 May 17;78:103802.
- Chazalon E, Conrath J, Ridings B, Matonti F. [Kyrieleis arteritis: report of two cases and literature review]. J Fr Ophtalmol. 2013;36(3):191-6.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

