CASE REPORT
A 55-year-old male was admitted to an ophthalmology clinic with a chief complaint of visual disturbances in his left eye.
He described a gradual decline in vision over recent months without any concurrent pain, redness, or discharge. The patient denied any history of trauma or systemic illnesses. Upon examination, visual acuity revealed 20/20 in the right eye (OD) and 20/50 in the left eye (OS).
Slit-lamp examination showed no abnormalities in the right eye (OD), while the left eye (OS) exhibited no conjunctival injection, a clear cornea, and no evidence of uveitis.
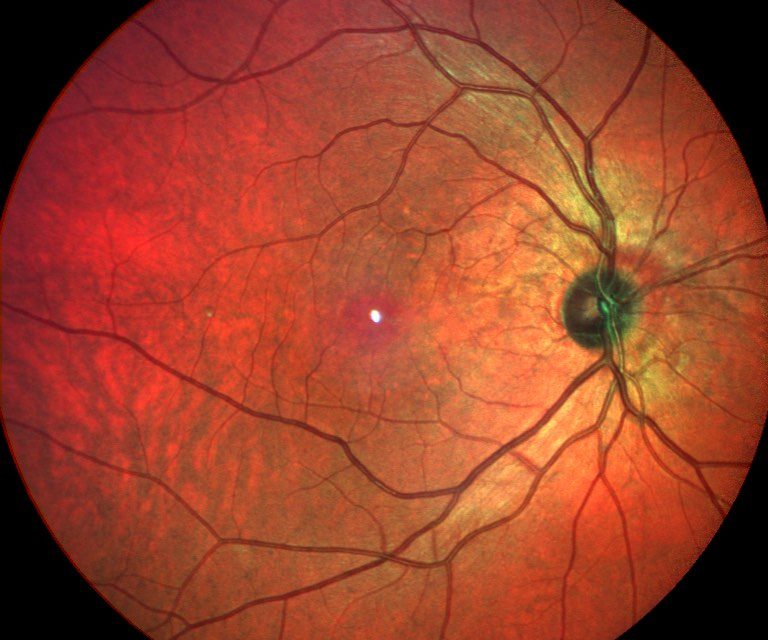
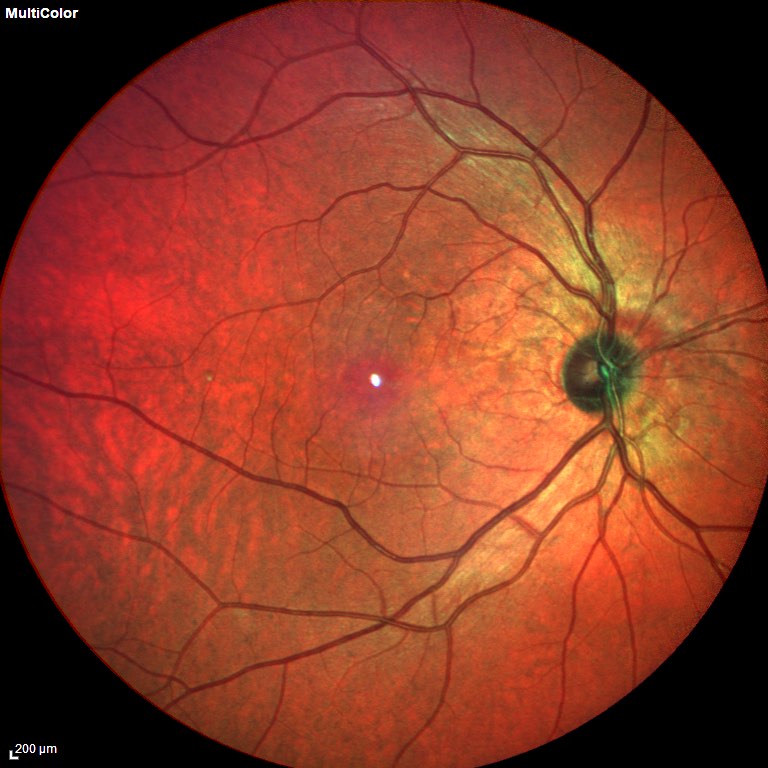
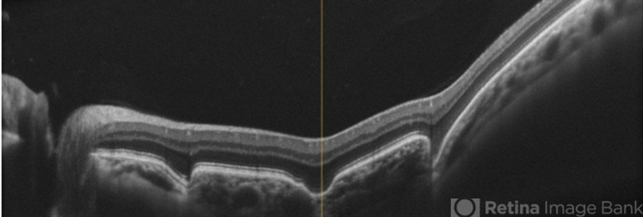
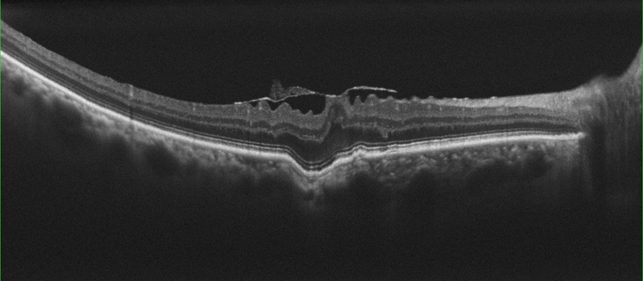
Fundus examination of the right eye (OD) displayed a normal optic disc, macula, and retinal periphery. In contrast, the left eye (OS) exhibited a localized area of retinal elevation and ellipsoid zone disruption at the macula, approximately 1 disc diameter in size, with no associated subretinal fluid or hemorrhage.
Optical Coherence Tomography (OCT) revealed normal retinal and choroidal anatomy in the right eye (OD) but showed Focal Choroidal Excavation (FCE) corresponding to the area of retinal elevation seen on fundus examination in the left eye (OS), with an ill-defined choroid-sclera interface in the affected region.
Consequently, the patient received a diagnosis of Focal Choroidal Excavation (FCE) in the left eye.
Focal Choroidal Excavation (FCE) DISEASE entity
Focal Choroidal Excavation (FCE) is a newly recognized clinical entity that is often incidentally found and presents asymptomatic or with mildly decreased visual acuity in the affected eye.
It has characteristic findings on optical coherence tomography (OCT) that can be used to distinguish it from other retinal lesions that may appear similar on ophthalmoscopy.
Focal Choroidal Excavation (FCE) was first described by Jampol in 2006 and coined as a term by Margolis in 2011.
It refers to a concavity of the choroid without local scleral changes that are often identified through a characteristic appearance on optical coherence tomography (OCT). This finding usually presents unilaterally and is found incidentally on exams, though exceptions to these patterns have been reported.
The majority of FCEs are thought to be congenital; however, the etiopathology of FCE remains a subject of active investigation.

While most instances of FCE remain relatively stable over time and are managed with close observation, several complications requiring intervention, such as choroidal neovascularization and serous detachment, have been described.
The precise etiopathology of Focal Choroidal Excavation (FCE) remains to date unclear. It has been suggested that the clinical entity may represent a common morphological manifestation of multiple processes, which may be either congenital or secondarily acquired.
Congenital FCE are thought to be mostly stationary and not likely to be vision threatening, while secondary FCE may be related to a variety of conditions — including pachychoroid disease, chorioretinal inflammation, retinal dystrophies, and malignancy — which may require treatment to prevent complications and disease progression.
In one study of patients aged <40 years old, only 3/1697 (0.18%) of eyes examined were found to have an FCE.
Focal Choroidal Excavation (FCE) MANAGEMENT
In cases of asymptomatic Focal Choroidal Excavation (FCE) without associated choroidal neovascular changes, observation without treatment is recommended.
A slow increase in concavity size on OCT may be observed, but changes to concavity size might also be noted due to unavoidable variability in imaging modality such as slice orientation.
Some authors have postulated that focal scar contraction and maturation may be responsible for the slow progression in concavity size observed in patients over time.
If there is evidence of lesion expansion or scleral thickening, a full evaluation for secondary causes of FCE should be undertaken to determine if any underlying process can be directly treated. For scleral thinning, surgical reinforcement of the sclera can be considered.
Additional complications may arise that require treatment, including secondary neovascularization and/or serous retinal detachment.
If encountered, these may be managed depending on lesion location and sequelae, with anti-VEGF agents, verteporfin photodynamic therapy, or focal laser photocoagulation.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Jampol, L. M. et al. Diagnostic and therapeutic challenges. Retina 26, 1072–1076 (2006).
- Margolis, R. et al. The expanded spectrum of focal choroidal excavation. Arch. Ophthalmol. 129, 1320–1325 (2011).
- Braimah, I. Z., Rapole, S., Dumpala, S. & Chhablani, J. Focal Choroidal Excavation in Retinal Dystrophies. Semin. Ophthalmol. 33, 161–166 (2018).
- Shinojima, A., Kawamura, A., Mori, R. & Yuzawa, M. Morphologic features of focal choroidal excavation on spectral domain optical coherence tomography with simultaneous angiography. Retina 34, 1407–1414 (2014).
- Obata, R. et al. Tomographic and angiographic characteristics of eyes with macular focal choroidal excavation. Retina 33, 1201–1210 (2013).
- Verma, S. et al. Focal choroidal excavation: review of literature. Br. J. Ophthalmol. 105, 1043–1048 (2021).
- Shah, R. C., Gopalakrishnan, M., Goyal, A., Anantharaman, G. & Sethia, A. Focal choroidal excavation: Cause or effect? Indian J. Ophthalmol. 67, 696–698 (2019).
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE