CASE REPORT
A 72-year-old male presented to the emergency department with blunt trauma to the eye. The right eye was unaffected and normal in appearance. The patient complained of reduced vision in the left eye with no pain or photopsia.
The patient had no significant past ocular history and was slightly myopic. His medical history revealed lung cancer and heart disease, including coronary stent surgery four years earlier. Hence it was noted that the patient’s medications list included two anticoagulants acetylsalicylic acid and clopidogrel bisulfate.
Upon initial ocular examination, no orbital bruising was seen around the left eye. Left visual acuity (VA) without correction was 6/24, improving to 6/18 with pinhole and right VA was 6/5.
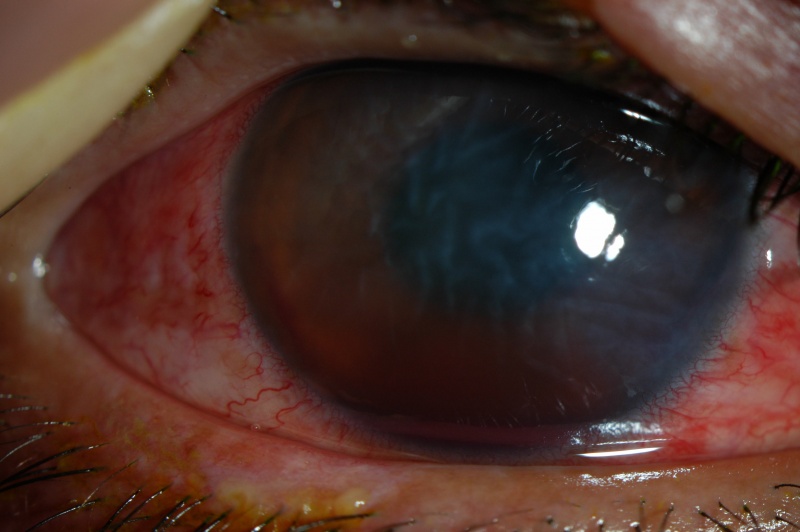
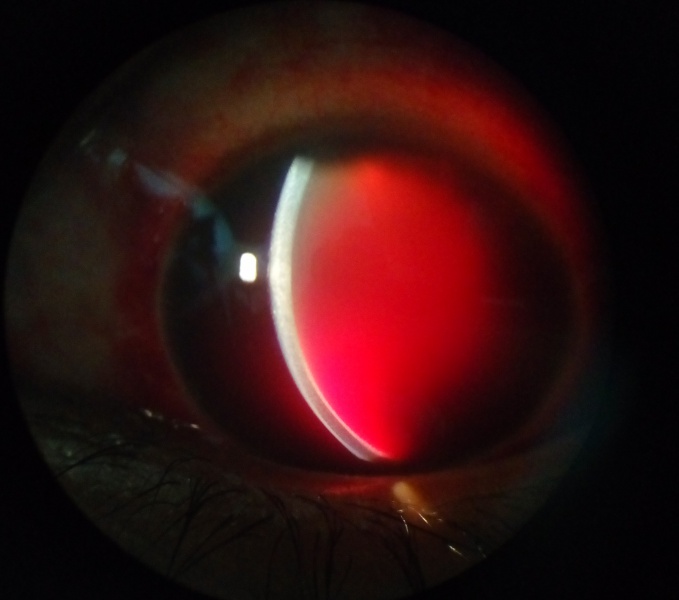
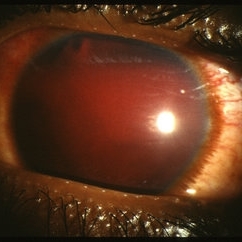
A slit lamp examination showed the left anterior chamber had a 60% hyphema with 4+ red blood cells, the pupil was round and no epithelial defects were seen. TonoPen intraocular pressure (IOP) was 18mmHg in the right eye and 26mmHg in the left.
Examination of the left fundus was not possible due to the presence of the hyphema hence a B-scan was performed. There was no evidence of peripheral vascular disease, retinal detachment vitreous hemorrhage. The patient’s diagnosis was a left Hyphema.
Hyphema: DISEASE entity
Hyphema is an accumulation of red blood cells within the anterior chamber. A small amount of blood that is only evident under close microscopic examination is referred to as a micro hyphema.

A majority of patients present with a history that correlates to the etiology. A history of trauma or recent ocular surgery is the most common risk factor.
However, a seemingly spontaneous hyphema can result at times from other causes. Despite the degree or etiology, the management of a hyphema and its associated complications can be challenging for any ophthalmologist.
Hyphema can occur after blunt or lacerating trauma, after intraocular surgery, spontaneously (e.g., in conditions such as rubeosis iridis, juvenile xanthogranuloma, iris melanoma, myotonic dystrophy, keratoiritis (e.g., herpes zoster), leukemia, hemophilia, von Willebrand disease, and in association with the use of substances that alter platelet or thrombin function (e.g., ethanol, aspirin, warfarin).
Blunt trauma is the most common cause of hyphema. Compressive force to the globe can result in injury to the iris, ciliary body, trabecular meshwork, and associated vasculature. The shearing forces from the injury can tear these vessels and result in the accumulation of red blood cells within the anterior chamber.
Hyphemas can also be iatrogenic in nature. Intraoperative or postoperative hyphema is a well-known complication of any ocular surgery. Rarely, the placement of an intraocular lens within the anterior chamber can result in chronic inflammation, secondary iris neovascularization, and recurrent hyphemas, known as uveitis-glaucoma-hyphema (UGH) syndrome.
This is a direct result of a malpositioned or rotating anterior chamber intraocular lens. This condition has also been reported in the posterior chamber, sulcus, and suture-fixated intraocular lenses.
Hyphema MANAGEMENT
Uncomplicated hyphemas should be managed conservatively, with an eye shield, limited activity, and head elevation. A patient should be monitored closely during the first few days after the injury as this is the highest risk time frame for rebleeding.
Maintaining head elevation of at least 45 degrees will allow the hyphema to settle inferiorly within the anterior chamber. This avoids central visual obstruction, as well as limits both corneal endothelial and trabecular meshwork exposure to red blood cells.
Most patients can be managed in an outpatient setting with close follow-up to evaluate vision, hyphema regression, and intraocular pressure.
However, hospitalization should be considered for non-compliant patients, patients with bleeding diathesis or blood dyscrasia, patients with severe ocular or orbital injuries, and patients with concomitant intraocular pressure elevations with known sickle cell disease.
Pain control for all patients with a hyphema should not include aspirin-containing products or NSAIDs, as these can increase the risk of further bleeding.
Medical Management:
Medical treatment for an isolated hyphema typically is topical. Topical corticosteroids (systemic for severe cases) may reduce associated inflammation, although the effect on the risk for rebleeding is debatable. Topical cycloplegic agents are also useful for patients with significant ciliary spasms or photophobia.
Systemic and topical aminocaproic acid (ACA) has been recommended in various studies as a treatment option to avoid secondary hemorrhage in hyphema patients.
If secondary hemorrhages are the result of lysis and retraction of a clot that has produced an occlusion of the traumatized vessel, then prevention of normally occurring clot lysis for 5-6 days should be advantageous to allow the injured blood vessel to more completely repair its integrity.
Tranexamic acid (TA) is another alternative. It is more potent than aminocaproic acid with fewer side effects.
If the intraocular pressure is not adequately controlled with medical management, or the patient develops further ocular complications (corneal blood staining, rebleed), surgical treatment may be necessary.
Surgical management:
A majority of hyphemas will resolve with medical management alone. Approximately 5 percent of patients with traumatic hyphema require surgery. The patient can typically be monitored for the first 4 days with medical treatment alone to allow for spontaneous resolution.
After that point, surgical intervention may be indicated in the setting of uncontrolled glaucoma, corneal blood staining, the persistence of a large or total hyphema, and active bleeding in the anterior chamber.
Uncontrolled intraocular hypertension is defined as greater than or equal to 50 mmHg for more than five days, or more than 25 mmHg for more than 24 hours in patients with sickle hemoglobinopathy despite maximal medical therapy.
Options for surgical intervention consist of anterior chamber irrigation and aspiration through a small incision (anterior chamber washout), hyphema evacuation with closed vitrectomy instrumentation, or clot irrigation with a filtering procedure (trabeculectomy).
Additionally, an anterior chamber paracentesis can be performed for temporizing control of elevated intraocular pressure. If a total hyphema is present, it’s possible that pupillary block could occur, and a peripheral iridectomy may be indicated during the time of surgery.
An anterior chamber washout with irrigation and aspiration is commonly performed first. If intraocular pressure remains uncontrolled, a trabeculectomy along with repeat anterior chamber washout is indicated.
Postoperative hyphemas may be seen at the time of surgery or within the first 2-3 days after surgery. If bleeding is identified intraoperatively, it must be identified and coagulated if it does not cease on its own.
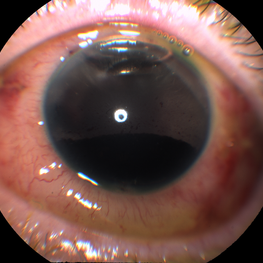
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Walton W, et al. Management of traumatic hyphema. Survey of Ophthalmology. 2002 Jul-Aug; 47(4): 297-334.
- Basic and Clinical Science Course. Glaucoma. pp 114-116; 2009-10.
- Condon, Garry P. Single-Piece Syndrome. Glaucoma Today. June 2011.
- Sheppard, John D. Jr, et al. Hyphema. Medscape Reference. 2009.
- Nasrullah A, Kerr NC: Sickle cell as a risk factor for secondary hemorrhage in children with traumatic hyphema. Am J Ophthalmol. 123:783-790. 1997.
- Bazzaz S, Katz JL, Myers JS. Post-Traumatic Glaucoma. In: Shaarawy T, Sherwwod MB, Hitchings RA, Crowston JG, eds. Glaucoma: Medical Diagnosis and Therapy. Elsevier:2009:431-439.
- Coles WH. Traumatic hyphema: an analysis of 235 cases. South Med J. 61:813-816. 1968.
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE


I’d like to find out more? I’d love to find out more details.