CASE STUDY
A 62-year-old male presented to an ophthalmology clinic with a chief complaint of sudden onset floaters and flashes in his left eye over the past week.
The patient described the floaters as dark specks that moved with his eye movements and occasional flashes of light, particularly noticeable in dim lighting conditions.
His medical history included hypertension managed with amlodipine and hyperlipidemia treated with atorvastatin. There were no prior ocular surgeries or significant trauma reported.
On examination, the patient had 20/20 vision in both eyes with correction. Anterior segment examination revealed clear corneas and lenses.
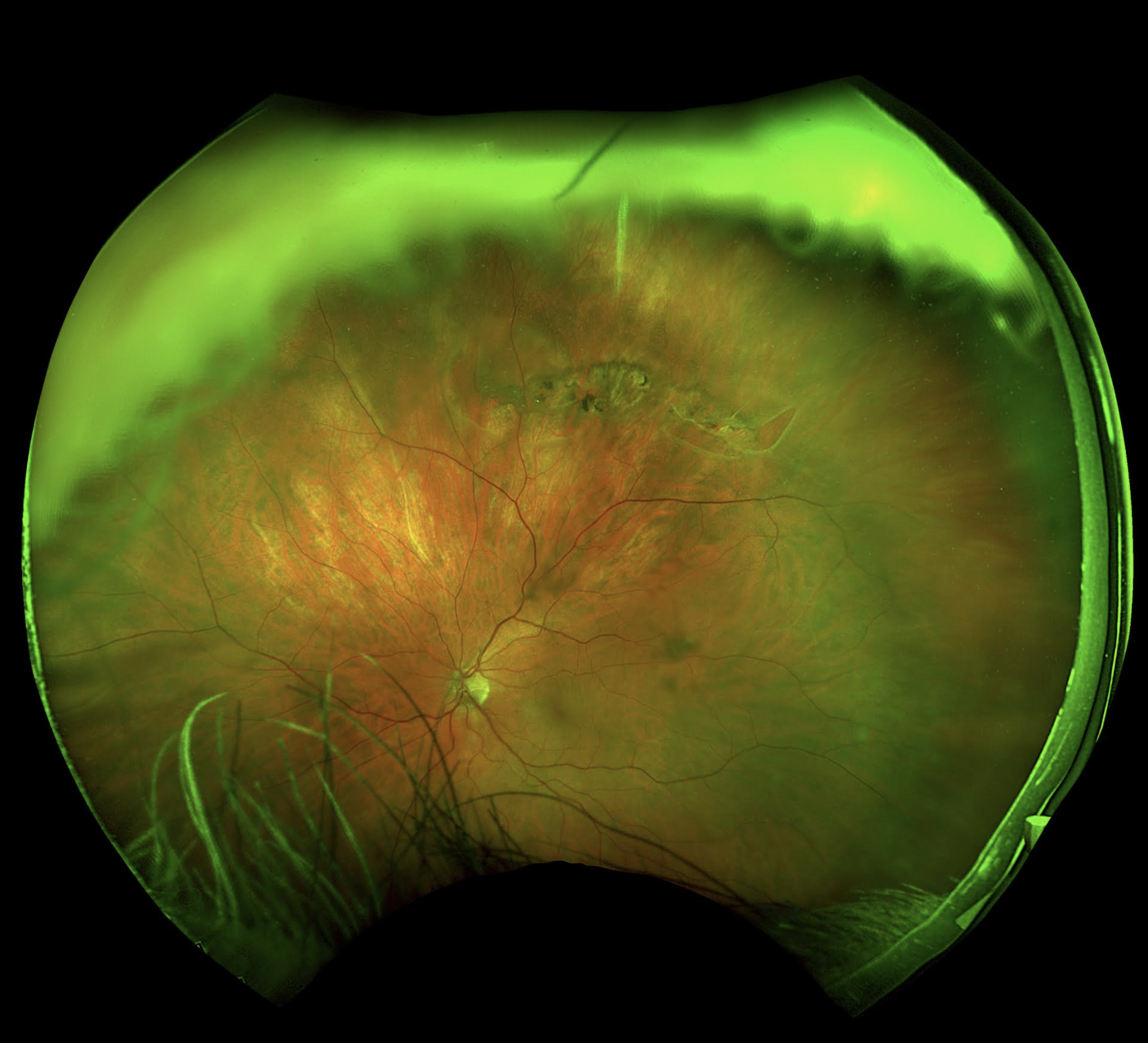
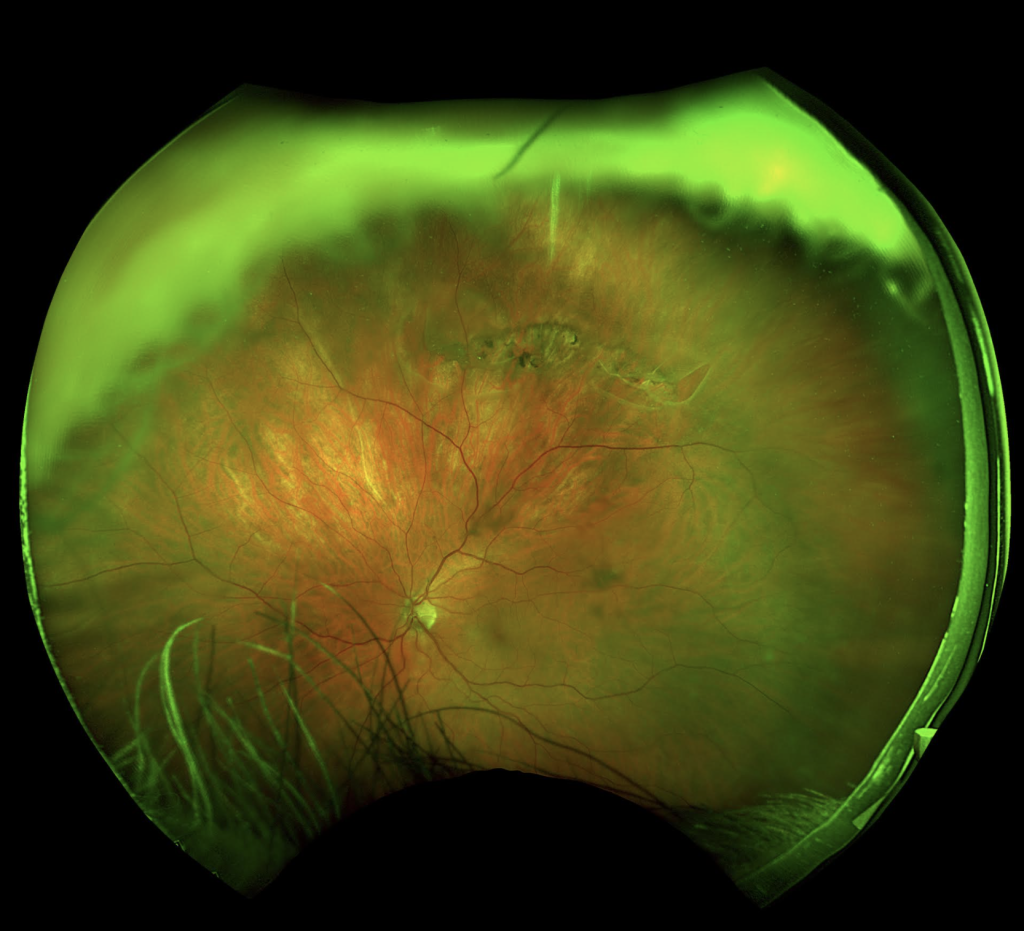
Posterior segment examination of the left eye showed vitreous floaters and a Weiss ring, with a normal retina and optic disc. The examination of the right eye was unremarkable. A diagnosis of Posterior vitreous detachment (PVD) was made.
POSTERIOR VITREOUS DETACHMENT (PVD)
Posterior vitreous detachment (PVD) is a common age-related condition characterized by the separation of the vitreous gel from the retina at the back of the eye.
This detachment occurs due to age-related changes in the vitreous structure, where the vitreous gel undergoes liquefaction and contraction. As it pulls away from the retina, symptoms such as floaters and flashes may occur.
Epidemiology
Posterior vitreous detachment (PVD) primarily affects individuals over the age of 50, although it can occur earlier in cases of trauma or myopia. The condition is equally prevalent in both genders and increases in frequency with age.
Clinical Features: Patients with PVD typically present with:
- Floaters: These are caused by clumps of collagen fibers or cellular debris within the vitreous casting shadows on the retina. They appear as spots, lines, or cobwebs that move with eye movements.
- Flashes of Light: Photopsia, or flashes of light, occur due to mechanical stimulation of the retina by the detached vitreous.
- Weiss Ring: A circular or horseshoe-shaped floater caused by vitreous detachment from the optic nerve head, often seen as a ring-shaped shadow in the visual field.
Diagnosis
Diagnosis of Posterior vitreous detachment (PVD) is primarily clinical, relying on patient history and examination findings.
Key diagnostic features include the presence of floaters, flashes of light, and visualization of a Weiss ring during fundoscopic examination.
Differential Diagnosis
Posterior vitreous detachment (PVD) should be differentiated from other causes of floaters and flashes, including:
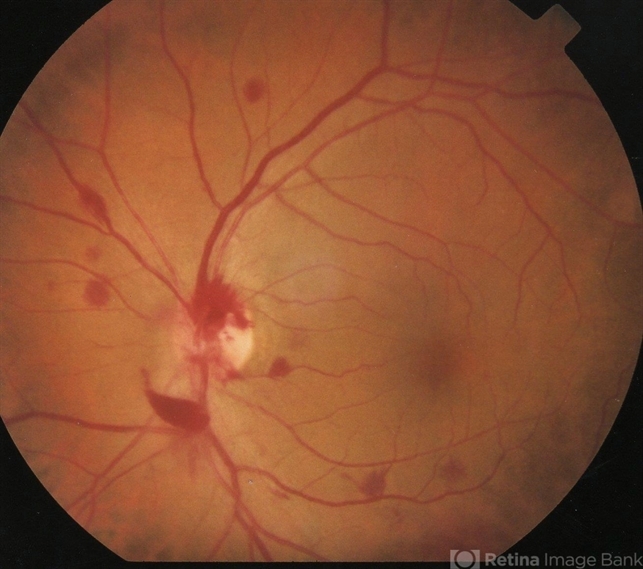
- Retinal Detachment: Urgent evaluation is crucial to distinguish PVD from retinal detachment, which requires immediate treatment.
- Vitreous Hemorrhage: Bleeding into the vitreous cavity can mimic Posterior vitreous detachment (PVD) symptoms and requires assessment for the underlying cause.
- Retinal Tears: These can also present with floaters and flashes and may progress to retinal detachment if untreated.
Management
Management of PVD is generally conservative, focusing on patient education and reassurance due to the benign nature of most cases.
Patients should be informed about the expected course of floaters and flashes, which typically improve over time as the brain adapts to ignore these visual disturbances.
Treatment Options: While specific treatment for Posterior vitreous detachment (PVD) itself is usually unnecessary, patients should be monitored for complications such as retinal tears or detachment.
In cases where retinal tears are identified, laser therapy or cryotherapy may be indicated to prevent progression to retinal detachment.
Prognosis
The prognosis for uncomplicated PVD is favorable, with most patients experiencing resolution or improvement in symptoms over weeks to months.
Approximately 10-15% of patients may develop symptomatic retinal tears, which can be managed effectively with timely intervention.
Complications
Although rare, complications of PVD include:
- Retinal Tears and Detachment: These occur when the vitreous traction leads to tears in the retina, which can progress to detachment if untreated.
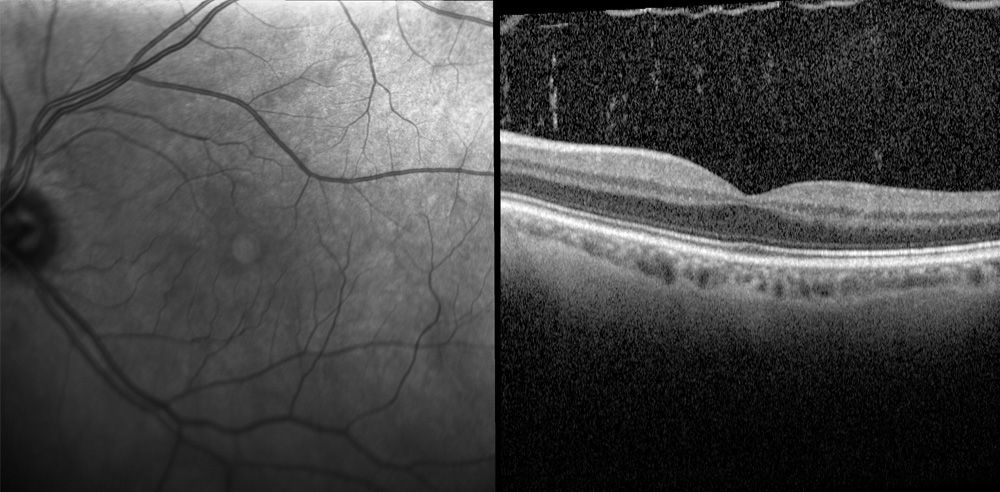
- Macular Hole: In some cases, persistent vitreous traction can lead to the formation of a macular hole, which may require surgical intervention.
Research and Future Directions
Ongoing research is exploring new imaging modalities and biomarkers to better understand the progression and risk factors associated with Posterior vitreous detachment (PVD).
Advances in vitreoretinal surgery techniques are also aimed at improving outcomes in cases requiring surgical intervention.
Conclusion
Posterior vitreous detachment is a common condition that primarily affects older adults and is characterized by the separation of the vitreous gel from the retina.
While typically benign, it is essential for clinicians to distinguish Posterior vitreous detachment (PVD) from more serious conditions like retinal detachment to ensure appropriate management and outcomes.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
References
- Johnson MW. Posterior vitreous detachment: evolution and complications of its early stages. Am J Ophthalmol. 2010;149(3):371-82.
- Sebag J. Anomalous posterior vitreous detachment: a unifying concept in vitreo-retinal disease. Graefes Arch Clin Exp Ophthalmol. 2004;242(8):690-8.
- Mitchell P, Smith W, Chey T, et al. Prevalence and associations of epiretinal membranes. The Blue Mountains Eye Study, Australia. Ophthalmology. 1997;104(6):1033-40.
- Spaide RF. Age-related choroidal atrophy. Am J Ophthalmol. 2009;147(5):801-10.
- Jackson TL, Donachie PH, Sparrow JM, et al. United Kingdom National Ophthalmology Database study of vitreoretinal surgery: report 1; case mix, complications, and cataract. Eye (Lond). 2013;27(5):644-51.
- Smiddy WE, Michels RG, Glaser BM, et al. Vitrectomy for floaters: prospective efficacy analyses and retrospective safety profile. Retina. 1998;18(3):205-10.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE