CASE REPORT
A 62-year-old female presented to an ophthalmology clinic with complaints of blurred central vision and distortion of straight lines in her left eye for the past two months.
She reported no trauma to the eye but had a history of hypertension and hypercholesterolemia, both of which were well-controlled with medications.
On examination, her visual acuity in the left eye was reduced to 20/80, while the right eye had a visual acuity of 20/25.
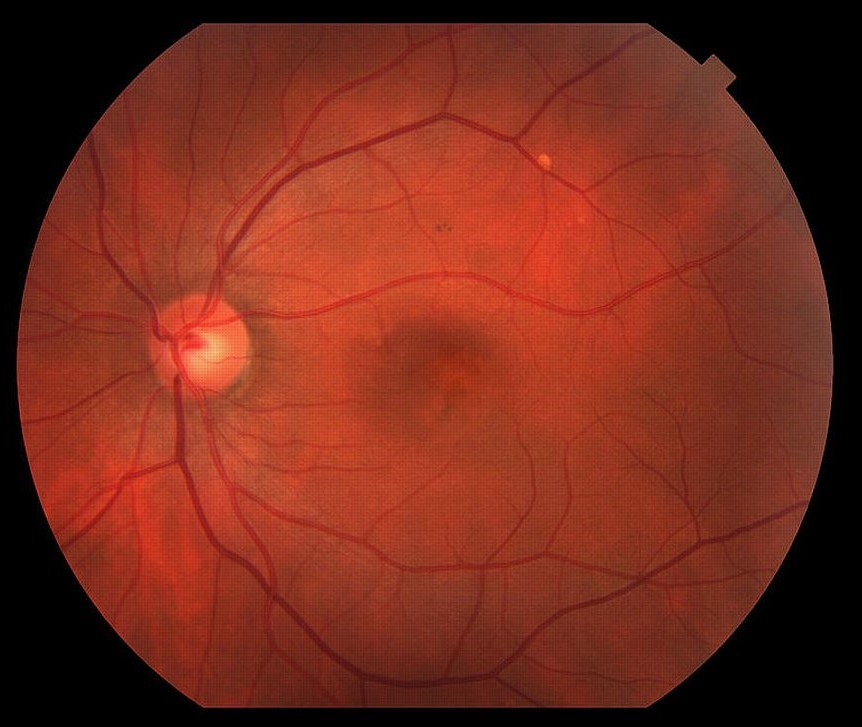
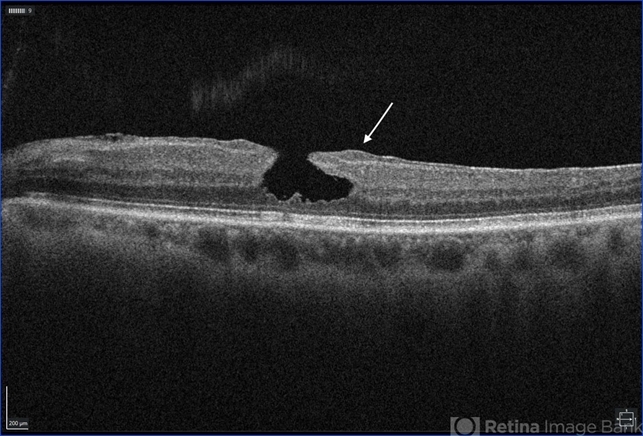
Intraocular pressure and anterior segment examination were within normal limits. Fundus examination revealed the presence of a lamellar macular hole.
Optical Coherence Tomography (OCT) imaging of the left eye showed characteristics consistent with a lamellar macular hole, including irregular foveal contour, separation of the neurosensory retina from the retinal pigment epithelium, and intraretinal cystic spaces.
Fluorescein Angiography (FA) was performed to confirm the diagnosis and rule out other macular pathologies.
DISEASE
Lamellar macular hole (LMH) is a retinal disorder that affects the macula involving a loss of tissue in the inner layers of the retina.
The majority of LMH cases are idiopathic. However, Lamellar macular hole (LMH) has been linked to conditions causing cystoid macular edema (CME) (e.g., Irvine-Gass syndrome, diabetic macular edema, retinal vein occlusions), as patients presenting such conditions may experience spontaneous rupture of the roof of a cystoid space.
Conditions involving tractional forces applied to the retina, such as presence of tractitional epiretinal membranes (ERM) or age-related vitreomacular tractions (VMT), are also considered risk factors.
Though the understanding of LMH has evolved with new optical coherence tomography (OCT) findings, it remains unclear whether all LMH form through tractional forces exerted on the fovea or through degeneration of the inner layers of the retina.
While initially described as a complication of CME, subsequent research identified conditions leading to the formation of LMH.
Partial or complete posterior vitreous detachment (PVD) causing traction on the fovea can potentially lead to the formation of intraretinal cysts/schisis or ERM (i.e., contractile preretinal proliferation of myofibroblasts with an extracellular matrix).
Lamellar macular hole (LMH) may also be the consequence of an aborted FTMH formation process. On the other hand, certain LMH do not exhibit apparent signs of traction.
Instead, they are rather associated to an epiretinal proliferation (ERP) of hyalocytes, fibroblasts, and glial cells lacking contractile properties and degeneration of the inner layers of the fovea; suggesting another subtype of LMH.
However, recent findings suggest that both the tractional and degenerative forms of LMH initially stem from a tractional force exerted onto retinal tissue.
MANAGEMENT
General treatment:
As most Lamellar macular hole (LMH) remain stable over time, no treatment is indicated in idiopathic, asymptomatic cases.
The treatment is surgical and consists of pars plana vitrectomy (PPV) which may involve the removal of preretinal tissue (ERM/ERP) and/or of the internal limiting membrane (ILM).
Medical therapy:
As of today, no therapeutic modalities/drugs are indicated for the treatment of idiopathic LMH. Patients are simply monitored until spontaneous closure occurs in certain cases or symptoms develop warranting surgical management.
Medical follow up:
Regular follow-up of LMH is essential to track the progression of the disease and consider surgical intervention if the LMH deteriorates over time, as they can progress to FTMH.
Surgery
Surgical treatment of LMH using PPV is usually indicated for patients with progressive deterioration of the foveal profile or symptomatic visual loss associated with metamorphopsia and/or central scotoma.
It remains that the decision to intervene surgically is made on a case-by-case basis, weighing risks and benefits for the patient.
PPV helps release vitreomacular adhesions by removing ERM/ERP and ILM, facilitating the restauration of a regular foveal profile.
Tamponade with air or gas may be used, but longer duration gas is not critical for the surgery to succeed. In those cases, patients are usually instructed to maintain prone positioning postoperatively.
Removal of the ERM/ERP and ILM has been shown to induce closure of the LMH, notably by releasing tractional forces.
However, peeling may be sometimes laborious, particularly with ERP which has a fluffy texture making it more difficult to peel.
Getting rid of the membrane around the LMH walls can lead to iatrogenic damage and the formation of FTMH postoperatively.
Alternative techniques include the use of platelet rich plasma during surgery, the fovea-sparing ILM peel, as well as the embedding of the peeled ILM into the LMH.
These approaches show promising results, as the articles in which they were described reported no cases of postoperative FTMH.
Surgical follow up
Regular surgical follow-ups are essential to assess for anatomical and functional success, as well as manage potential complications.

Complications
The most common surgical complication following PPV is cataract. Non-closure of Lamellar macular hole (LMH) and FTMH development are also reported.
Other complications include intraoperative retinal breaks, postoperative ocular hypertension or hypotension, and/or acute postoperative endophtalmitis.
Prognosis
Patients with LMH have a favorable prognosis, as most remain stable over time, with no significant visual acuity decline.
While not necessary, surgical treatment is effective with most studies reporting a statistically significant improvement in visual acuity postoperatively.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Frisina R, Pilotto E, Midena E. Lamellar Macular Hole: State of the Art. Ophthalmic Res. 2019;61(2):73-82. doi:10.1159/000494687.
- Denise Compera, Ricarda G Schumann, Matteo G Cereda, et al. Progression of lamellar hole-associated epiretinal proliferation and retinal changes during long-term follow-up. Br J Ophthalmol. 2018;102(1):84. doi:10.1136/bjophthalmol-2016-310128
- Wu L, Bradshaw R. Primary Lamellar Macular Holes: To Vit or Not to Vit. J Clin Med. 2022;11(17). doi:10.3390/jcm11175046
- Govetto A, Dacquay Y, Farajzadeh M, et al. Lamellar Macular Hole: Two Distinct Clinical Entities? Am J Ophthalmol. 2016;164:99-109. doi:10.1016/j.ajo.2016.02.008
- Lee CY, Hsia Y, Yang CM. Formation and evolution of idiopathic lamellar macular hole-a pilot study. BMC Ophthalmol. 2022;22(1):432. doi:10.1186/s12886-022-02669-4
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

