CASE REPORT
A 65-year-old male with a history of hypertension, hyperlipidemia, and a remote smoking habit presented with a complaint of progressive visual impairment in the left eye over the past six months, accompanied by intermittent episodes of dull, aching pain around the left eye and decreased visual acuity.
On examination, his best-corrected visual acuity (BCVA) was 20/30 in the right eye and 20/200 in the left eye, with a marked afferent pupillary defect in the left eye.
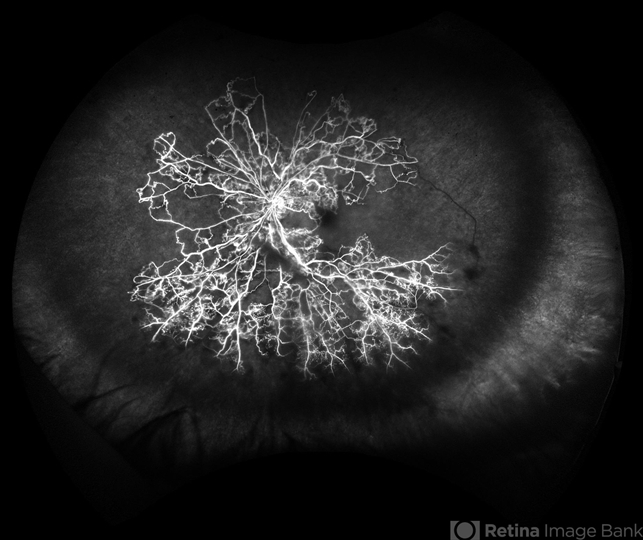
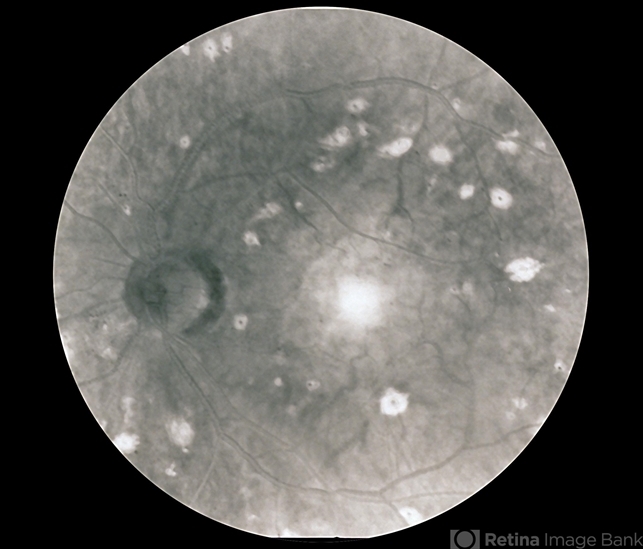
Intraocular pressure (IOP) measurements were normal, and anterior segment examination revealed no abnormalities. Fundus examination of the left eye revealed dilated, tortuous retinal veins, retinal hemorrhages, cotton-wool spots, and macular edema, while the right eye appeared normal, indicative of ischemic retinopathy.
Diagnostic workup included color Doppler ultrasound revealing significant (70%) stenosis of the left internal carotid artery, fluorescein angiography confirming impaired blood flow to the retina, brain MRI with contrast ruling out cerebral infarctions but confirming carotid artery stenosis, and comprehensive blood tests assessing underlying systemic conditions contributing to Ocular ischemic syndrome (OIS).
Based on these findings, the patient was diagnosed with Ocular ischemic syndrome (OIS).
Ocular Ischemic Syndrome (OIS) DISEASE entity
Ocular ischemic syndrome (OIS) is a rare, but vision-threatening condition associated with severe carotid artery occlusive disease (stenosis or occlusion) leading to ocular hypoperfusion.
Principal symptoms include visual loss, transient visual loss, and ischemic ocular pain. OIS commonly occurs in the elderly with men more affected than women, owing to the higher incidence of atherosclerosis and carotid artery disease in these patients.
OIS has important systemic implications, as a disease of the common (CCA) or internal (ICA) carotid arteries may cause ipsilateral ocular signs and symptoms that in turn could herald a cerebral infarction.

Ocular Ischemic Syndrome (OIS) MANAGEMENT
The management of Ocular ischemic syndrome (OIS) involves a multidisciplinary approach. The aim is threefold, firstly to treat the ocular complications and prevent further damage, secondly to investigate and treat the associated vascular risk factors, and third to perform vascular surgery whenever indicated.
The ocular treatment is directed toward control of anterior segment inflammation, retinal ischemia, increased IOP, and neovascular glaucoma.
Topical therapy includes steroids to suppress anterior segment inflammation and cycloplegics to stabilize the blood–aqueous barrier and limit iris movement in order to decrease the likelihood of a spontaneous hyphema.
Medical treatment of increased IOP consists of ocular hypotensive agents that reduce aqueous outflow (topical β-adrenergic blockers, or α-agonists that also increase uveoscleral flow), along with topical and/or oral carbonic anhydrase inhibitors.
Prostaglandins, pilocarpine, and other anticholinergic agents should be avoided whenever possible because they may increase ocular inflammation.
When neovascular glaucoma develops, IOP control is usually refractory to medical therapy and surgery (trabeculectomy with antimetabolites or aqueous shunt implants), or diode laser cyclophotocoagulation is often required.
In patients with no useful vision and in pain who are thought to have limited potential for visual recovery, cycloablation is a viable option. If the eye remains painful, retrobulbar injection of alcohol or chlorpromazine may provide relief.
If these fail to alleviate pain in a blind eye, enucleation or evisceration should be considered. Panretinal photocoagulation may be effective in some patients with ocular neovascularization caused by carotid occlusive disease and may prevent the development of neovascular glaucoma.
In eyes with poor fundus visualization, 360° transconjunctival cryotherapy or transscleral diode laser retinopexy may be considered.
Intravitreal anti-vascular endothelial growth factor (bevacizumab and ranibizumab) and triamcinolone have been used in the treatment of iris neovascularization and cystoid macular edema complicating Ocular ischemic syndrome (OIS).
Surgical Treatment
Carotid Artery Endarterectomy:
The NASCET trial established carotid endarterectomy (CEA) plus aspirin as superior to aspirin alone in preventing strokes in both symptomatic and asymptomatic carotid artery stenosis.
Current guidelines from the American Academy of Neurology and the American Heart Association/American Stroke Association recommend CEA for symptomatic stenosis of 50–99% with <6% perioperative risk, and for asymptomatic patients, CEA is advised for stenosis of 60–99% with <3% perioperative risk.
CEA effectively improves ocular blood flow and reduces ocular ischemia, as evidenced by increased peak systolic velocity in the ophthalmic artery post-surgery, potentially alleviating hypotensive retinopathy and lowering stroke risk.
However, iris neovascularization may limit visual recovery, reducing the beneficial impact of CEA on visual acuity.

Carotid Artery Stenting:
Endovascular carotid artery stenting (CAS) is a treatment alternative for patients who need CEA. CAS has been used for patients who are considered to be at high risk for complications after CEA including those with anatomic conditions rendering surgery technically difficult, such as previous neck irradiation or radical neck surgery, recurrent stenosis after CEA, contralateral recurrent laryngeal-nerve palsy, tracheostomy, and carotid stenosis above the C2 vertebral body.
Medical conditions that increase the risk of surgery, such as unstable angina, recent myocardial infarction, multivessel coronary disease, and congestive heart failure, are also indications for CAS.
Carotid artery stenting has been shown to improve the ocular blood flow in patients with acute and chronic forms of Ocular ischemic syndrome (OIS).
Extracranial–Intracranial (EC-IC) Arterial Bypass Surgery
EC-IC bypass surgery involves the surgical anastomosis of the superficial temporal artery (STA) with a branch of the middle cerebral artery (MCA).
It is indicated when there is complete occlusion of the ICA or the CCA or when ICA stenosis is inaccessible (at or above the C2 vertebral body) to CEA.
The aim is to increase cerebral blood flow and prevent the development of cerebral ischemia. CEA usually improves ocular hemodynamic parameters, but stabilization or improvement in vision seems to occur only when performed early before the development of iris neovascularization or neovascular glaucoma.
Carotid endarterectomy is also beneficial in preventing cerebral infarctions. A multidisciplinary approach is essential when considering surgery in patients with OIS factoring in the patient’s anatomic considerations and associated co-morbidities.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Gordon N. Ocular manifestations of internal carotid artery occlusion. The British journal of ophthalmology. May 1959;43(5):257-267.
- Hedges TR, Jr. Ophthalmoscopic findings in internal carotid artery occlusion. American journal of ophthalmology. May 1963;55:1007-1012.
- Bullock JD, Falter RT, Downing JE, Snyder HE. Ischemic ophthalmia secondary to an ophthalmic artery occlusion. American journal of ophthalmology. Sep 1972;74(3):486-493.
- Biousse V. Carotid disease and the eye. Current opinion in ophthalmology. Dec 1997;8(6):16-26.
- Brown GC, Magargal LE. The ocular ischemic syndrome. Clinical, fluorescein angiographic, and carotid angiographic features. International ophthalmology. Feb 1988;11(4):239-251.
- Kearns TP, Siekert RG, Sundt TM, Jr. The ocular aspects of bypass surgery of the carotid artery. Mayo Clinic proceedings. Mayo Clinic. Jan 1979;54(1):3-11.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

