CASE REPORT
A 56-year-old woman presented complaining of blurry vision in both eyes and black spots in the lower field of her left eye for 4 days. She denied flashing lights, eye or neck pain, fever, chills, or a new neurologic deficit. Several mosquitoes had bitten her in the previous 3 weeks.
She admitted to nausea, extreme malaise, muscle weakness, and soreness. On examination, Her uncorrected visual acuities were 20/25 OD and 20/30 OS. Intraocular pressure was 17 mm Hg in each eye.
Dilated fundus examination revealed bilateral mild nonproliferative diabetic retinopathy and no evidence of chorioretinal infiltrates.
She returned to the emergency department 5 days later with progressive blurring of vision in both eyes and black spots also now in the right eye. Visual acuities were 20/25 OD and 20/40 OS. Her intraocular pressure was elevated to 23 mm Hg in the right eye and 32 mm Hg in the left eye.
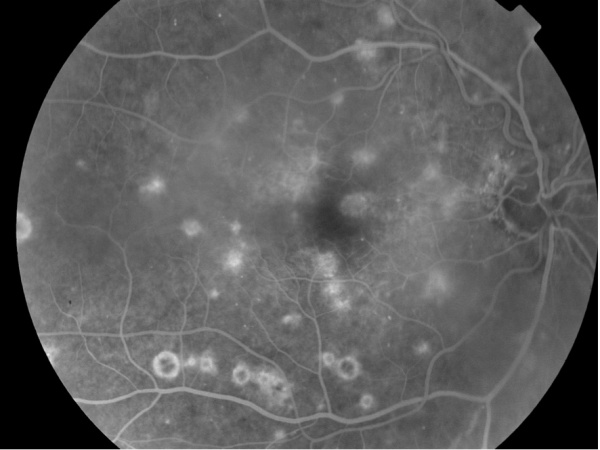
Slitlamp examination and dilated smartphone fundoscopy demonstrated trace conjunctival hyperemia, bilateral nongranulomatous keratic precipitates, and moderate anterior chamber and anterior vitreous inflammation. West Nile virus serologies were positive by enzyme-linked immunosorbent assay. A diagnosis of West Nile Retinopathy was confirmed.
West Nile Retinopathy DISEASE entity
West Nile virus retinopathy is a subtype of multifocal chorioretinitis caused by the West Nile virus. The West Nile virus (WNV) is a single-stranded RNA flavivirus of the Japanese encephalitis serogroup.

It is a zoonotic disease most commonly transmitted by the bite of the Culex genus of mosquitoes (especially Culex pipiens). WNV reservoirs are wild birds though horses and humans act as “dead-end” hosts (Figure 1).
Alternate routes of human infection have been documented in the case of blood transfusions, organ transplants, exposure in a laboratory setting, and vertically during pregnancy. However, the vast majority of cases of WNV infection have been from infected mosquitoes.
West Nile Retinopathy Diagnostic procedures
Fluorescein angiography may demonstrate early hypofluorescence and late staining of active lesions and central hypofluorescence and peripheral hyperfluorescence of inactive lesions.
Indocyanine green angiography typically demonstrates more lesions than can be appreciated by fluorescein angiography.
Autofluorescence may highlight the old scars better than fundus examination of fundus photographs.

West Nile Retinopathy MANAGEMENT
General treatment
There is currently no proven treatment for WNV infection. For systemic infection, therapy consists of supportive treatment. In severe cases, hospitalization for the administration of intravenous fluids and respiratory support may be necessary.
Should choroidal neovascularization occur, anti-VEGF therapy may be warranted.
Complications
Through rather uncommon, complications from intraocular WNV infection may occur in the form of chorioretinal scars, choroidal neovascularization, vitreous hemorrhage, tractional retinal detachment, ischemic maculopathy, optic atrophy, and retrogeniculate damage.
Prevention
Primary prevention of infection is the mainstay of WNV infection control. Wearing protective clothing, using mosquito repellent, and using mosquito larvicides are proven strategies for decreasing the incidence of infection.
A vaccine for WNV is currently under development but has not gone through clinical trials.

Prognosis
The prognosis for WNV retinopathy is very good. In the vast majority of cases, the ocular disease is self-limited, and visual acuity returns to baseline.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
1. Bakri SJ, Kaiser PK. Ocular manifestations of west nile virus. Curr Opin Ophthalmol. 2004; 15:537-540.
2. Davis LE, DeBiasi R, Goade DE, et al. West nile virus neuroinvasive disease. Ann Neurol. 2006; 60:286-300.
3. Garg S, Jampol LM. Systemic and intraocular manifestations of west nile virus infection. Surv Ophthalmol. 2005; 50:3-13.
4. Glass WG, Lim JK, Cholera R, Pletnev AG, Gao JL, Murphy PM. Chemokine receptor CCR5 promotes leukocyte trafficking to the brain and survival in west nile virus infection. J Exp Med. 2005; 202:1087-1098.
5. Glass WG, McDermott DH, Lim JK, et al. CCR5 deficiency increases risk of symptomatic west nile virus infection. J Exp Med. 2006; 203:35-40.
6. Khairallah M, Ben Yahia S, Ladjimi A, et al. Chorioretinal involvement in patients with west nile virus infection. Ophthalmology. 2004; 111:2065-2070.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

