CASE REPORT
A 14-year-old patient crushed the left side of his face against the back window of an automobile. He did not lose consciousness after the trauma.
He was examined by a neuro pediatrician on the same day and had normal neurological status. The patient presented for an ophthalmologic examination six days after the trauma because of a hematoma of his left upper eyelid.
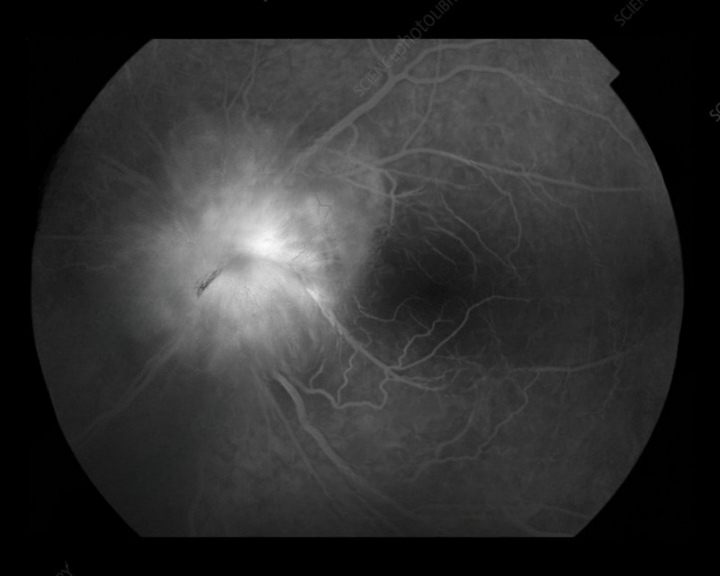
Visual acuity, intraocular pressure, bulbar motility, pupillary reaction, and slit-lamp biomicroscopy were normal. Smartphone fundus examination of the right eye was normal, but the left optic disk was elevated with blurred disk margins
Because of the trauma and the finding of the left-sided papilledema, the patient was referred for repeat neuropediatric examination and perimetry. These results were normal, so the patient was referred for multi-slice computed tomography (MSCT) scanning of the brain and orbits.
MSCT showed a .6-mm oblique hyperdense mass behind the left optic disk, which was described as probably buried disk drusen. Ultrasonography confirmed deeply buried optic disk drusen of the left optic disk, which could not be seen on ophthalmologic examination. The diagnosis of unilateral pseudopapilledema was made
DISEASE
Pseudopapilledema is defined as an anomalous elevation of one or both optic discs without edema of the retinal nerve fiber layer.
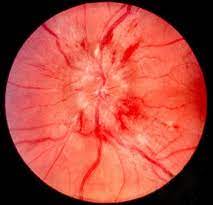
Papilledema, on the other hand, is a swelling of the optic disc due to increased intracranial pressure. It is important to distinguish pseudopapilledema from true papilledema, which can be the first sign of the disease process with the potential for vision loss, neurological impairment, or death.
Patients thought to have papilledema are often subjected to lumbar puncture, MRI, and extensive laboratory studies to find the underlying cause. In this article, we will cover multiple causes of pseudopapilledema and how to differentiate them from true papilledema.
Diagnosis
Fundus examination
The distinction between true papilledema and pseudopapilledema can sometimes be made on the basis of ophthalmoscopic findings. In true papilledema, swelling of the peripapillary nerve fiber layer causes an obscured view of underlying retinal vessels.
The appearance of vessels in the peripapillary nerve fiber layer is the most important distinguishing feature between pseudopapilledema and papilledema. Splinter hemorrhages may also be seen in true papilledema. Spontaneous venous pulsations (SVPs), a reassuring sign that there is no raised intracranial pressure, may also indicate pseudopapilledema.
However, SVPs may be absent in up to 10% of normal individuals. Peripapillary subretinal hemorrhages often signify pseudopapilledema. Optic disc drusen may show a “lumpy bumpy” disc appearance with visible retinal vessels.
Diseases associated with optic disc drusen may present with characteristic physical exam findings. For example, patients with retinitis pigmentosa may have waxy pallor of the nerve, attenuated vessels, and peripheral bone spicules; patients with pseudoxanthoma elasticum can have angioid streaks and peau d’orange skin changes; and patients with Alagille syndrome will present with a characteristic facial appearance.
MANAGEMENT
Distinguishing papilledema from pseudopapilledema can be tricky, but is important to avoid invasive and unnecessary workup for increased intracranial pressure.
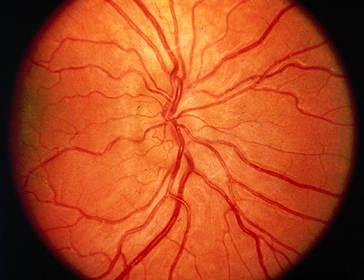
Anomalies suggestive of pseudopapilledema can be suspected when any elevated, noncongested disc is seen with no physiologic cup, and with nondilated veins and arteries passing over its surface.
Patients with optic disc anomalies are recommended to be evaluated frequently by an ophthalmologist, who will monitor for changes such as hemorrhages of the disc or enlargement of scotomas.

If the disc anomalies are unchanging and pseudopapilledema is established, the patient can be informed about that to avoid future medical confusion. Management of pseudopapilledema varies by etiology. Patients with systemic disorders should be managed appropriately for their symptoms.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- American Academy of Ophthalmology. Pseudopapilledema and papilledema.
- Hoyt, WF, Pont, ME. Pseudopapilledema: Anomalous Elevation of the Optic Disk. JAMA. 1962;181(3):191-196. doi:10.1001/jama.1962.03050290013003
- Miller, NR, Newman, NJ, Biousse, V, Kerrison, JB, et al. Walsh and Hoyt’s Clinical Neuro-Ophthalmology Sixth edition. 2005;1(6).
- Auw-Haedrich C, Staubach F, Witschel H. Optic disk drusen. Surv Ophthalmol. 2002;47(6):515-32
- Freund P, Margolin E. Pseudopapilledema. StatPearls Publishing. 2019 Jan.
- El-Koofy NM, El-Mahdy R, Fahmy ME, et al. Alagille syndrome: clinical and ocular pathognomonic features. Eur J Ophthalmol. 2011;21(2);199-206.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

