DISEASE
Vitreous wick syndrome, vitreous tug syndrome, or vitreous touch syndrome, is characterized by vitreous bands or strands to the corneal wound which can be associated with cystoid macular edema (Irvine-Gass Syndrome).
Vitreous wick syndrome occurs after eye surgery or trauma and is characterized by microscopic wound breakdown accompanied by vitreous prolapse that develops into a vitreous ‘wick’.
At first, vitreous wick syndrome was limited to anterior-segment procedures. Subsequently, however, posterior fistulous tracts with vitreous entrapment were reported after vitreoretinal surgery. Vitreous wick syndrome has also been identified as a potential cause of endophthalmitis after intravitreal injection of triamcinolone through the pars plana.
With the rise of intravitreal drug delivery devices currently available, vitreous wick syndrome may become more common.
Vitreous wick syndrome may result from the following situations:
- Routine cataract surgery with unrecognized posterior capsular rupture or zonular dehiscence with vitreous prolapse and adhesion to the surgical wound
- Complicated cataract surgery with posterior capsular rupture and inadequate anterior vitrectomy with adhesion to the surgical wound
- Transconjunctival/transscleral intravitreal injection of pharmacologic agents
- Sutureless small-gauge pars plana vitrectomy
- Inadequate prolapsed vitreous removal during repair of scleral or sclerocorneal lacerations or scleral melts
MANAGEMENT
Vitreous wick syndrome treatment is primarily surgical but may also include medical therapy as appropriate. The surgical approach to the management of this syndrome depends on the presentation (without any restrictions on diet indicated). Participation in strenuous activities and contact sports should be restricted until recovery is complete.
Medical therapy
The type of topical antibiotics used in the treatment of vitreous wick syndrome depends on the suspected infecting agent or the culture and sensitivity results.
In cases of endophthalmitis, medical therapy is initiated and selected according to its effectiveness against the suspected or confirmed (via culture and sensitivity results) infecting agents. Subconjunctival and intravitreal antibiotics should be given (and pars plana vitrectomy should be considered alongside medical therapy).
Surgical procedures
Laser therapy
Patient Preparation
Explain the procedure beforehand to the patient and obtain informed consent. Remind the patient the procedure often requires more than one session.
When the vitreous strand or band passes through the pupil, treatment is often facilitated by the administration of pilocarpine 2% every 10 minutes for 3 or 4 drops preoperatively. Inducing the stretch of the vitreous through miosis facilitates identification of the strand. When the laser transects the strand the release of tension is shown more definitively.
Postoperative laser care
Strong topical steroids (eg, prednisolone acetate 1% or dexamethasone 0.01%) are given 4 times daily until visual improvement occurs, typically in 2 to 3 months. Topical nonsteroidal anti-inflammatory drugs may be of benefit alone or with topical steroids.

Ketorolac or diclofenac drops are usually administered 4 times daily. The addition of a systemic nonsteroidal anti-inflammatory drug can be considered in recalcitrant cases.
IOP elevation following vitreolysis has not been well documented. A beta-blocker or brimonidine drops at the time of treatment probably provide adequate prophylaxis.
Prophylactic Vitreolysis
With the availability of laser vitreolysis, the surgeon may treat vitreous strands of the wound in the absence of cystoid macular edema (CME) in an effort to prevent its later development. Only a large, long-term randomized treatment trial can determine the usefulness of this approach. Some patients with vitreous strands to the wound never acquire CME.
A baseline fluorescein angiogram and optical coherence tomography may be done to document the macular status in patients with vitreous to the wound and good visual acuity. If CME is detected, laser vitreolysis is probably indicated even in good acuity. If visual loss later develops with the new onset of CME, the baseline angiogram will be useful to further support therapeutic intervention.
Surgery
The precise surgical treatment varies with the circumstances. The following is a generalized procedural description.

Initially, the vitreous wick is excised or severed with Vannas-type scissors by lifting the exposed vitreous strand with a cotton-tipped applicator or fine nontoothed forceps. Alternatively, a suction-cutting instrument inserted into the anterior chamber may be used.
Vitrectomy may be performed via an anterior limbal or closed posterior approach. It is imperative that no vitreous strand is left above the pupillary plane. To detect any remaining vitreous, one should sweep the anterior chamber with a spatula from a paracentesis site 90° away from the surgical wound.
Intracameral injection of pupil constrictors (carbachol intraocular solution) may help pull any remaining anterior-chamber vitreous wick back into the posterior segment. Intracameral preservative-free triamcinolone acetonide may help visualize vitreous strands.
A mobile (reacting), well-centered round pupil suggests clearance from any vitreous that is invading the anterior chamber. Adequate surgical closure is accomplished with nylon 10-0 sutures.
The patient is discharged on a regimen of topical antibiotics, either broad-spectrum or targeted on the basis of culture and sensitivity results.
Nonsteroidal anti-inflammatory drugs (NSAID)-containing ophthalmic drops are given to decrease cystoid macular edema and steroid drops are given to decrease inflammation.
Pilocarpine ophthalmic drops are given to maintain pupillary constriction and prevent anterior segment migration of posterior vitreous during the acute healing phase.
Patients should receive follow-up care 1-2 days after surgery. If this initial follow-up examination identifies no problems, regular checkups should be scheduled for uneventful anterior segment surgeries.
The use of an eye shield, especially at night, protects the globe from any untoward traumatic episodes.
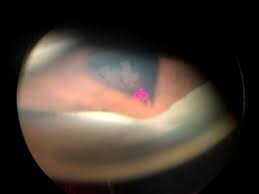
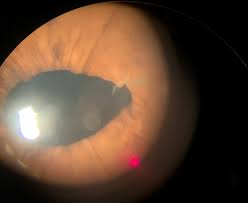
HOW TO TAKE SLIT-LAMP EXAM IMAGES WITH A SMARTPHONE?
Smartphone slit-lamp photography is the new advancement in the field of science and technology in which photographs of the desired slit-lamp finding can be taken with smartphones by using the slit-lamp adapters.
Slit-lamp Smartphone photography
REFERENCES
- Iliff CE. Treatment of the vitreous-tug syndrome. Am J Ophthalmol. 1966 Nov;62(5):856-9.
- Chen SD, Mohammed Q, Bowling B, Patel CK. Vitreous wick syndrome–a potential cause of endophthalmitis after intravitreal injection of triamcinolone through the pars plana. Am J Ophthalmol. 2004 Jun. 137(6):1159-60; author reply 1160-1.
- Ruiz RS, Teeters VW. The vitreous wick syndrome. A late complication following cataract extraction. Am J Ophthalmol. 1970 Oct. 70(4):483-90.
- Neetens A, Rubbens MC, Smets RM. Vitreous wick syndrome. Bull Soc Belge Ophtalmol. 1987. 223 Pt 2:41-5.
- Couch SM, Bakri SJ. Use of triamcinolone during vitrectomy surgery to visualize membranes and vitreous. Clin Ophthalmol. 2008 Dec. 2(4):891-6.
- Schmidt JC, Chofflet J, Hörle S, Mennel S, Meyer CH. Three simple approaches to visualize the transparent vitreous cortex during vitreoretinal surgery. Dev Ophthalmol. 2008. 42:35-42.
Slit-lamp Smartphone photography

RETINAL IMAGING BY YOUR SMARTPHONE


The articles you write help me a lot and I like the topic