CASE REPORT
A 27-year-old male patient was admitted to a hospital with 2 days history of giddiness, vomiting, abdominal pain, and difficulty in breathing. He was a recently diagnosed diabetic (Type 1) on ayurvedic treatment.
Physical examination showed him to be drowsy, dyspneic, dehydrated, and with other features suggestive of diabetic ketoacidosis (DKA). He had no cutaneous or tendinous xanthomas or xanthelasmas. He had no visual disturbances.
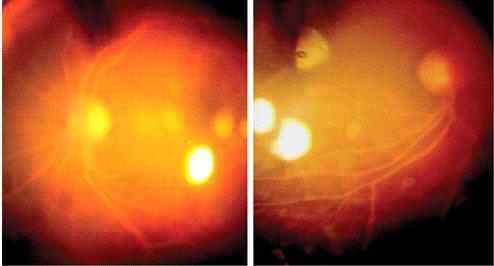
On Day 1, the fundus was examined for diabetic retinopathy in the ward and it revealed that vessels in the posterior pole and peripheral area of each eye had a creamy appearance. Both arterioles and veins were flat and ribbon-like and their color was salmon pink around the disc and creamy milk white in the periphery.
The optic disc and macula were normal and there was no evidence of diabetic retinopathy. Fundus examination confirmed the same finding of lipemia retinalis.
Lipemia retinalis description
As you know diabetes affects the retina resulting in diabetic retinopathy, and hypertension affects the retina resulting in hypertensive retinopathy, in the same way, hypertriglyceridemia (chylomicronemia) also damages the retina resulting in lipemia retinalis.
Lipemia retinalis is a feature of chylomicronemia syndrome.
- When plasma triglycerides level exceeds 2000 mg/dl then it leads to lipemia retinalis.
- It is mostly diagnosed in patients who come for a check-up of their lipid abnormalities.
- It is also diagnosed in infants and neonates who have come for their screening and treatment of Retinopathy of Prematurity (ROP).
Secondary causes:
These include
- Uncontrolled Diabetes
- Endocrine diseases (hypothyroidism, obesity, hypercortisolism, metabolic disorders )
- Renal diseases(Renal dialysis, renal failure)
- Pregnancy
- Medications (Corticosteroids, estrogen, antipsychotics)
- Liver disease(Acute hepatitis)
- Dietary intake(a diet rich in unsaturated fats and carbohydrates, excessive intake of alcohol)
- Systemic diseases (HIV infections, spinal cord injury, and organ transplant)

Symptoms:
Most of the time, patients are asymptomatic, but sometimes Decreased visual acuity is also noted.
Signs:
Creamy white color of retinal vessels.
Grading:
Grade I:
- It is an early stage in which peripheral retinal vessels get a creamy tint.
- In this stage, triglycerides level ranges from 2500 to 3499 mg/dl.
Grade II:
- It is a moderate stage in which creamy discoloration from the peripheral area extends toward the central retina including the optic disc.
- In this stage, triglycerides level ranges from 3500 to 5000 mg/dl.
Grade III:
- It is a marked stage in which the whole fundus gets salmon color and all vessels become Creamy thus making arteries and veins indistinguishable.
- Triglycerides level is >5000 mg/dl in this stage.
MANAGEMENT of Lipemia retinalis
Lipemia retinalis is a temporary occurring condition that sometimes resolves on its own.
The main treatment is to manage the risk factor which in the present case is hypertriglyceridemia. It can be managed with medication, exercise, and dietary modifications. In infants with lipemia retinalis, a low fat diet without breast milk is advised.
Medical Treatment:
As such there is no medical treatment, only cholesterol and triglycerides-lowering drugs are given which can help in lowering the serum triglycerides level below 500 mg/dl.
These drugs include
- Fibrate (fibric acid derivatives)
- n-3 polyunsaturated fatty acids (fish oil)
- Nicotinic acid
Surgical Treatment:
Normally surgery is not advised in this condition. But in the case of severe hypertriglyceridemia, an exchange transfusion can be done.
Prognosis:
Its prognosis is good. Once the main risk factor is kept under control, all the signs and symptoms of this disease vanish and the patient’s condition gets normal.
Complications:
After recovery from Lipemia retinalis, these patients are at increased risk of Coronary artery disease, stroke, myocardial infarction, retinal artery and vein occlusion, and retinal ischemia, so they should be kept on regular follow-up.
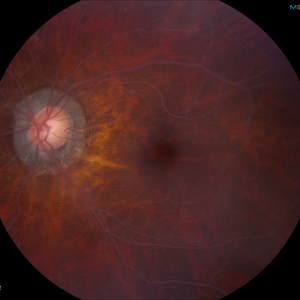
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Zahavi A, Snir M, Kella YR. Lipemia retinalis: case report and review of the literature. J AAPOS. 2013 Feb;17(1):110-1.
- Heyl AG. Intra-Ocular Lipæmia. Trans Am Ophthalmol Soc. 1880;3:54-66.
- Vinger PF, Sachs BA. Ocular manifestations of hyperlipoproteinemia. Am J Ophthalmol. 1970 Oct;70(4):563-73.
- Rayner S, Lee N, Leslie D, Thompson G. Lipaemia retinalis: a question of chylomicrons? Eye (Lond). 1996;10 ( Pt 5):603-8.
- Brunzell JD, Bierman EL . Chylomicronaemia syndrome: interaction of genetic and acquired hypertriglyceridemia. Med Clin North Am 1982;66:455–68.Chait A, et al. Chylomicronaemia syndrome in diabetes mellitus. Diabetes Care 1981;4:343–8.
- Chase LA. Diabetic lipaemia retinalis. Can Med Assoc J 1927;17:197–204.
- Jain A, Mochi TB, Braganza SD, Agrawal S, Shetty BK, Pachiyappan B. Lipemia retinalis in an infant treated for retinopathy of prematurity. J AAPOS. 2017 Jun;21(3):254-257.

RETINAL IMAGING BY YOUR SMARTPHONE

