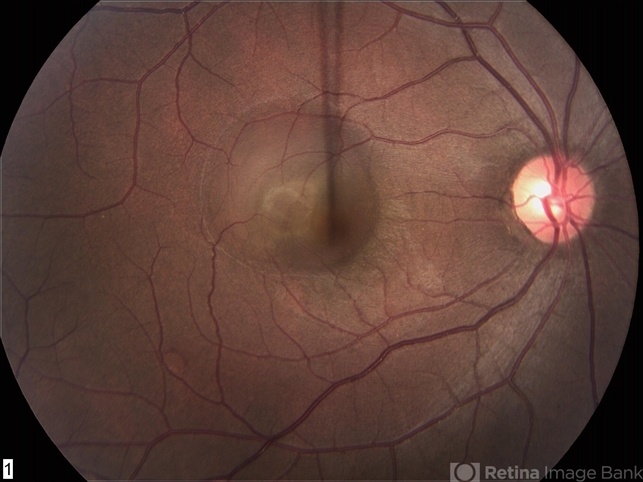
Central serous chorioretinopathy, commonly referred to as CSC, is a condition in which fluid accumulates under the retina, causing a serious (fluid-filled) detachment and vision loss.
CSC most often occurs in young and middle-aged adults. For unknown reasons, men develop this condition more commonly than women. Vision loss is usually temporary but sometimes can become chronic or recur.

Medical Therapy
Anti-corticosteroid therapy:
As mineralocorticoid receptor action has been implicated in the pathogenesis of CSCR, Zhao, and Bousquet treated patients with eplerenone, a mineralocorticoid antagonist, for five weeks and found a significant and rapid improvement of retinal detachment with improvement in mean central macular thickness, sub-retinal fluid height, and visual acuity that persisted at five months follow up.
Similar studies have supported this potential treatment and have shown greater efficacy in patients with chronic CSCR.
Spironolactone, another anti-corticosteroid, has been shown to decrease sub-retinal fluid, decrease central retinal thickness, and increase BCVA in patients with chronic CSCR.
A prospective, randomized, double-blind, and placebo-controlled study with a crossover design showed a reduction in sub-retinal fluid and sub-foveal choroidal thickness.
A prospective, randomized, placebo-controlled trial studying the use of eplerenone for chronic CSCR found modest gains in BCVA and improvement in sub-retinal fluid height (in press).
Mineralocorticoid antagonists may raise serum potassium levels, especially in patients with congestive heart failure and chronic kidney disease.
Hyperkalemia can manifest as fatigue, muscle weakness, palpitations, and arrhythmias. Before starting a medication in this class, reviewing medical history and discussing it with the primary care doctor is recommended.
Baseline serum potassium levels and renal function should be established, such as with a basic metabolic panel. Initiation of medication should be postponed or avoided if serum potassium concentration is >5.5 mEq/L, creatinine clearance is <50 mL/min, or serum creatinine is >2 mg/dL in men and >1.8 mg/dL in women.
Other anti-corticosteroid treatments have also been studied. Finasteride, a 5a-reductase inhibitor with anti-androgenic properties, was shown to improve central macular thickness (CMT) and sub-retinal volume in a study of five patients but these findings reversed when the drug was discontinued.
Mifepristone, an anti-progesterone and anti-glucocorticoid agent, was shown in a study of 16 patients to improve Snellen’s visual acuity.
Rifampin, an anti-tuberculous drug, and cytochrome P450 3A4 inducer, accelerates the metabolism of steroids and has been shown to benefit patients with CSCR.
However, its use may be avoided in countries with a high prevalence of tuberculosis due to the risk of resistance.
A case study of a patient with multifocal CSCR with persistent SRF of two years who was treated with rifampin showed complete resolution of SRF in one month.
Side effects of rifampin include orange-colored body fluids, anorexia, and hepatotoxicity.
Melatonin is an endogenous neuromodulator linked to circadian cycles and sleep regulation, aging, and neuroprotection via an antioxidant mechanism.
Melatonin also inhibits corticosteroids and has a minimal side effect profile, making it a target for CSCR treatment. A study of eight patients showed significant improvements in CMT (87.5%) and BCVA (100%) compared to controls. Furthermore, no side effects were observed.
Aspirin
Low-dose aspirin has been explored in treating CSCR. Elevated levels of plasminogen activator inhibitor 1 (PAI 1), a marker of platelet aggregation, have been linked to steroid use and have been measured in patients with CSCR.
A prospective study of 113 eyes with CSCR showed faster improvement in BCVA compared to control.
Helicobacter pylori treatment
A randomized control trial (RCT) of patients who tested positive for H. pylori studied the effect of treatment of H. pylori treatment of chronic CSCR.
This study found that patients treated for H. pylori infection have faster resolution of sub-retinal fluid (9 weeks) versus control (11 weeks) but no change in BCVA.
A case series of treated biopsy-positive H. pylori patients showed resolution of SRF in 14 of 15 patients. However, another RCT tested the same hypothesis and found no statistical change in the resolution of SRF and BCVA.
Dang and colleagues did find a statistically significant improvement in foveal sensitivity in the H. pylori treatment group. These studies with contradictory results indicate that larger RCTs are needed to elucidate the clinical significance of H. pylori treatment on the resolution of CSCR.
Anti-adrenergic agents
The role of anti-adrenergic therapy for CSCR is unclear. A small case series in 1993 described 6 patients with CSCR treated with metoprolol, a non-selective beta-blocker, who improved symptomatically and had partial or complete resolution of retinal detachment.
Other studies have shown that both metipranolol (non-selective beta-blocker) and metoprolol tartrate (selective beta-1 blocker) induced remission of CSCR.

In contrast, a randomized controlled double-blind study examining the impact of beta-blockade with metipranolol throughout acute CSCR found no difference in the course of acute CSCR between the beta-blocker group and the control group.
Since this RCT examined patients with acute CSCR, the conclusions are not readily applicable to patients with chronic CSCR.
Although anti-adrenergic agents are beneficial in CSCR in some studies, this therapy has not been widely implemented in treatment.
Intravitreal anti-VEGF therapy
The use of anti-vascular endothelial growth factor (VEGF) agents is based on the idea that VEGF levels may be elevated due to the choroidal pathology.
However, studies have shown that VEGF levels are similar between CSCR patients and control patients. A meta-analysis of four controlled studies with patients treated with intravitreal bevacizumab (IVB) compared to control showed no improvement in BCVA or CMT at six months. Of note, patients with coexisting choroidal neovascularization and CSCR (confirmed on FA or OCT-angiography) do benefit from anti-VEGF therapy.
Also, polypoidal choroidal vasculopathy which is an important differential of CSCR in patients older than 50 years, may benefit from anti-VEGF agents.
Surgical Management
Laser Photocoagulation
Patients who show persistent visual defects or lack of improvement in imaging after a few months may require alternative therapies.

One option is laser photocoagulation, including focal argon laser and micropulse diode laser photocoagulation. Both rely on angiography to identify focal targets based on hyperfluorescence at sites of RPE detachment/disruption.
It is hypothesized that the destruction of these detached sites allows scarring that re-attaches the retina. During this process, healthy surrounding RPE cells can pump SRF back into the choroid and expedite healing.
For patients with focal RPE detachments not involving the fovea, focal argon laser photocoagulation may be considered.
It has been shown to reduce the duration of CSCR by up to two months, with complete resolution of RPE detachment and increased speed of improvement of VA. However, the long-term benefits of focal argon laser photocoagulation remain unclear.
Several studies showed significantly decreased rates of CSCR recurrence in treatment groups vs placebo groups after 9 to 18 months of follow-up.
Others have concluded there was no difference in CSCR recurrence rates between groups after 1 to 12 years of follow-up.
Although focal argon laser photocoagulation may lead to more rapid resorption of SRF and recovery of VA, patients should be made aware of its potential side effects. Because the laser destroys targeted retinal tissue, patients may develop symptomatic scotomas corresponding to these sites.
Choroidal neovascularization (CNV) and further vision loss can result if Bruch’s membrane is ruptured by the laser, requiring additional therapy.
Due to these potential complications, patients treated with focal argon laser photocoagulation should have regular ophthalmology follow-up.
Photodynamic therapy
Photodynamic therapy (PDT) with verteporfin, a photosensitizer that accumulates in vessels and helps target therapy, causes endothelial damage and vascular hypoperfusion to inhibit the choroidal hyperpermeability seen in CSCR.
Several reports and studies have demonstrated that PDT can be used in chronic CSCR patients to decrease SRF and improve BCVA.
Unfavorable side effects, which include choroidal ischemia, RPE atrophy, RPE rip, retinal thinning, and secondary choroidal neovascular membrane (CNVM) have led to the development of safer versions of PDT, which are reduced-dose PDT and reduced-fluence PDT.
Bae demonstrated that reduced-fluence PDT was superior to intravitreal ranibizumab in an RCT for improving BCVA and central retinal thickness.
Half-dose PDT versus half-fluence PDT was compared in eyes with chronic CSCR, demonstrating that half-dose PDT treatment allowed for faster SRF resolution and decreased recurrence compared to half-fluence PDT.
Further studies titrating the dosage of verteporfin and laser fluence are needed to more precisely compare safety profiles and efficacy. PDT necessitates the avoidance of physical activity after treatment.
PDT may be used for subfoveal or diffuse leaks in CSCR.
Subthreshold Micropulse Laser Photocoagulation
The traditional argon laser is thought to work by activating the RPE cells at the periphery of the laser burn that is affected but not destroyed by thermal energy.
Subthreshold micropulse laser (SML), also known as “high-density, low-intensity” laser, uses subthreshold energy that selectively targets RPE cells without inducing chorioretinal damage or scarring.
This allows exposure to a large area of RPE cells, which then down-regulate cytokine production and inflammation. The laser is applied in pulses at a frequency that allows heat dissipation to prevent structural heat damage to the retina.
Unlike conventional lasers, SML can be safely applied to the fovea. Fluorescein angiography and indocyanine green (ICG) angiography can be supplemented to determine areas of treatment.
Several wavelengths of pulse lasers including green 532 nm laser, yellow 577 nm laser, and infrared 810 nm laser have been used to target different cells in the retina.
For example, the 577 nm yellow laser has the highest hemoglobin-to-melanin ratio making it the best SML for vascular structures.
Furthermore, the 577 nm laser allows for more concentrated light with a lower power compared to the 810 nm laser. Several uncontrolled studies have shown the effectiveness of 810 nm and 577 nm SML therapy.
In an RCT, chronic CSCR patients treated with 810 nm SML showed significantly better BCVA, lack of scotoma, and improved contrast sensitivity compared to patients treated with argon laser photocoagulation.
A study comparing 577 nm SML with PDT in the treatment of chronic CSCR showed a better treatment response in the SML group and greater improvement in central retinal thickness in the SML group.
In addition to the superior outcomes with SML over PDT, SML avoids the potential side effects of PDT such as RPE atrophy, choroidal neovascularization, choriocapillary ischemia, and transient reduction of macular function.
Similar to PDT, there is no visible tissue response during treatment, which is why SML treatment guidelines for optimal laser, energy, and duty cycle parameters are a much-needed area of investigation.
Scleral resection
Venkatesh and colleagues have reported a resolution of exudative retinal detachment from chronic CSCR/ diffuse retinal pigment epitheliopathy after scleral resection.
This patient had a borderline low axial length of the eyeball and thick ocular coats on the ultrasonogram.
Would you have interest in taking retinal images with your smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
References
- Bousquet E, Beydoun T, Zhao M, Hassan L, Offret O, Behar-Cohen F. Mineralocorticoid Receptor Antagonism In The Treatment Of Chronic Central Serous Chorioretinopathy: A Pilot Study. Retina. 2013;33(10):2096-2102. doi:10.1097/IAE.0b013e318297a07a.
- Chin EK, Almeida DR, Roybal CN, et al. Oral mineralocorticoid antagonists for recalcitrant central serous chorioretinopathy. Clin Ophthalmol Auckl NZ. 2015;9:1449-1456. doi:10.2147/OPTH.S86778.
- Barnes PJ. Corticosteroid effects on cell signalling. Eur Respir J. 2006;27(2):413-426. doi:10.1183/09031936.06.00125404.
- Herold T, Prause K, Wolf A, Mayer W, Ulbig M. Spironolactone in the treatment of central serous chorioretinopathy–a case series. Graefes Arch Clin Exp Ophthalmol. 2014;252(12):1985–1991.
- Bousquet E, Beydoun T, Rothschild P-R, et al. Spironolactone for nonresolving central serous chorioretinopathy: a randomized controlled crossover study. Retina. 2015;35(12):2505–2515.
- Chrapek O, Spacková K, Rehák J. Treatment of central serous chorioretinopathy with beta blockers. Ceska Slov Oftalmol Cas Ceske Oftalmol Spolecnosti Slov Oftalmol Spolecnosti. 2002;58(6):382-386.
- Chrapek O, Jirkova B, Kandrnal V, Rehak J, Sin M. Treatment of central serous chorioretinopathy with beta-blocker metipranolol. Biomed Pap. March 2013. doi:10.5507/bp.2013.015.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE


Great content! Super high-quality! Keep it up!